-

Cutaneous Leishmaniasis in a Traveler: A Case Report
Sarah Al-Obaydi, Nemer Dabage, and James DeMaio
Leishmaniasis, a vector-borne infection transmitted by sandflies, is endemic throughout the Mediterranean basin and the tropics. We present a case diagnosed in Florida after overseas travel.
-

Pasteurella Multocida Bacteremia Secondary to Multiple Cat Scratches
Charles Boadu, Andrea Hernandez, Bassem Zeidan, John T. Young, and Johnathan Frunzi
Pasteurella multocida(P. multocida)is part of the normal gastrointestinal and upper respiratory flora of domestic and wild animals such as dogs, cats, rabbits, opossums, boars, tigers, lions and horses (1, 2). Transmission of P. multocidais usually through scratches and bites leading to infections of the soft tissue and skin (3,4). P. multocida bacteremia is rare, but occurs in individuals with major risk factors including chronic pulmonary disease, diabetes mellitus, end state renal disease (ESRD), and an immunocompromised state (3,4). Non traumatic infections of P. multocida in immunocompromised individuals,are more likely to require care in the intensive care unit (ICU), likely to occur in patients with severe comorbidities, and are likely to end in mortality (4). In this case, we present P. multocida bacteremia in an immunocompromised adult male with end stage kidney on hemodialysis.
-

Thinking Outside the Box in Liver Tox
Kimberly Brizell and Geoffrey L. Goldsberry
DILI is the most common cause of acute liver failure in the United States. However, it is important to consider that the agent at play may not be common to the United States. We aim to highlight the importance of using a "global mindset" when treating international and frequent traveling patients, but also demonstrate the severe hepatotoxic risks associated with Nimesulide.
-
What is Scannable? An MRI Safety Guide
Michael Burcescu, Ravi Patel, Robert Hessemer, Peter Lore, Sriharsha Kota, and Guarav Kumar
Supernumerary MRI protocols and recommendations exist to guide physicians at the forefront of patient care. While urgent imaging may be necessary for critical patients, inadvertent imaging of implantable devices can incur serious morbidity and mortality[11]. The American College of Radiology published a 30-page manual in 2013[1] on MRI safe practices and releases yearly updates with critical information separately[2]. There is increased utilization of advanced imaging modalities, especially among academic institutions[3]. Physicians are hard pressed to maximize efficiency; uncertainty delays imaging. Moreover, inappropriate orders delay appropriate management. We present pertinent and often questioned considerations in a comprehensible format along with devices that may have ferromagnetic material such as iron, cobalt, or nickel.
-

Pneumonia: An Unexpected Graveyard Visitor?
Daniel A. Casas, Jigar Chauhan, Melanie Williams, Jan Sambataro, David Sukhai, Pablo G. Dubon, and Jorge Perez
Community acquired pneumonia caused by Influenza can present with superinfection. On rare occasions, an unexpected organism is discovered.
-

Bedside Point of Care Ultrasound Diagnosing Bilateral Valve Involvement in Infective Endocarditis
Corey Cole, Alfredo Tirado, and Jonathan Schwadron
Endocarditis is a well known complication of intravenous drug abuse which classically affects the tricuspid valve. It is usually diagnosed by formal echocardiogram and positive blood cultures. Vegetations involving both the mitral and tricuspid valves are rare, occurring in less than 5% of all cases of infective endocarditis. 1 Here we report a case of a patient with vegetations on both valves which was discovered by point of care ultrasound.
-

A Rare Case of Primary Cutaneous Mucoepidermoid Carcinoma
Hassie Cooper, Maheera Farsi, Richard Miller, Pay Kamrani, and Dudith Pierre Victor
Mucoepidermoid carcinoma (MEC) is a well-documented malignant tumor commonly found in the salivary glands. Cutaneous involvement is very rare, especially when presenting as a primary cutaneous neoplasm. Gallagher first described primary cutaneous MEC in 1959 and since then, to the best of our knowledge, there have been approximately 20 reports published in the literature. Here we present a very rare case of primary cutaneous mucoepidermoid carcinoma.
-

The Difficult Airway: Developing a Consistent Approach
Catherine Divingian, Tammy Ferro, and Dudith Pierre-Victor
The primary objectives were to determine the best practices in managing difficult airways (DAs) and to generate a simplified algorithm for a consistent approach. Additional objectives included organizing a DA cart, and integrating the information into the electronic medical record (EMR).
-

Kounis Syndrome
Charles Doerner, Mark Sawh, Tamer A. Amer, and Konstantinos Marmagkiolis
Kounis syndrome, also known as allergic vasospastic angina, is a type of acute coronary syndrome caused by an allergic reaction or immune response to a substance.[1] It is essentially an “allergic angina” which is believed to be caused by mast cell activation and release of cytokines and histamine causing spasm of the artery leading to acute coronary syndrome and acute myocardial infarction. Stress cardiomyopathy (Takotsubo syndrome), which predominantly affects post-menopausal women, may also occur in anaphylaxis where transient ventricular dysfunction associated with regional ventricular wall abnormalities extending beyond the regions of coronary blood supply ensues.[2] The suspected prevalence of Kounis syndrome in the United states is 1.1% among those that were hospitalized for allergic, anaphylactic or hypersensitivity reactions [3]. Due to differences in management strategy, it is important to differentiate between Kounis syndrome and ACS due to other causes, especially in those with a history of coronary artery disease.
-

Cervical Cancer Recurrence in the Colon
Samantha A. Erb, Shreyash Pandya, and Johnny Johnson
Cervical cancer is the fourth leading cancer worldwide in women, ranking only after breast cancer, colorectal cancer, and lung cancer. Because it is typically diagnosed at a younger age compared to other major cancer types, it leads to a proportionally greater loss in life-years. Most cancers occur in squamo-columnar junction, the transition point between squamous and columnar cells; squamous cell carcinoma accounts for approximately 70% of cervical cancer cases. Treatment options vary depending on the stage at diagnosis and include surgery (conization or hysterectomy), radiation, chemotherapy, targeted therapy, and immunotherapy. Prognosis is affected by stage, tumor volume, age and performance status, and treatment type.
Local recurrence of cervical cancer is not uncommon. It is known to metastasize to distance sites including the lung, liver, bone, and supraclavicular lymph nodes, with rare cases involving the breast, paraspinal muscles and duodenum. Metastatic spread of cancer from extracolonic origin to the colon is uncommon. It occurs very rarely in breast and lung carcinomas (~2%), as well as stomach, prostate, breast, ovarian and melanoma This is a care case of a recurrence of cervical cancer that spread to the colon and presented as a sigmoid lesion.
-

Carcinoid Syndrome Arising from the Descending Colon causing Carcinoid Heart Disease
Julien A. Exposito, Adam Salomon, Oliver Fowler, Christopher Cooke, Joelle Ellis, Patricia Chun, and Christiano Caldeira
-

An Atypical Presentation of Neuroleptic Malignant Syndrome
Rudy Forte, Shiwani Kamath, Debra Angelo, and Johnathan Frunzi
Neuroleptic Malignant Syndrome (NMS) is a rare, but potentially life threatening condition associated with dopamine blockade, particularly first-generation antipsychotics. The complex pathophysiology of NMS remains somewhat unclear and debatable as the symptoms are not fully explained by dopamine blockade alone.1 D2 dopamine receptor antagonism remains responsible for most cases of NMS, however a few cases have been reported in which little to no D2 blockade activity was present.1
This poster is about an atypical presentation of NMS.
-

A Rare Case of Trichilemmal Carcinoma: Histology and Management
Lisa F. Fronek, Allyson Brahs, Maheera Farsi, and Richard Miller
Trichilemmal carcinoma (TC) is a rare, malignant, adnexal neoplasm that is derived from the outer root sheath (ORS) of the hair follicle. These tumors predominantly occur in elderly patients on sun-exposed areas, specifically on the head and neck with the face defined as the most common location. The mean age of diagnosis is 70 years old with a slight male predominance. These lesions are commonly identified as a papular, nodular, and sometimes, exophytic. They generally arise de-novo, but may also derivate from an underlying proliferating trichilemmal cyst with a loss of p53, a seborrheic keratosis, a nevus sebaceous, or a scar. They can be locally aggressive and may exhibit telangiectasias and ulceration due to local destruction.
While the clinical differential diagnosis commonly includes basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and keratoacanthoma, the histopathological differential also includes trichilemmoma, trichoepithelioma, clear cell SCC, clear cell porocarcinoma, and clear cell hidradenocarcinoma. The main differentiating histological feature in a TC is the evidence of trichilemmal keratinization, where the tumor exhibits an absence of granular layer between the stratum spinosum and stratum corneum. The standard of treatment for TC is wide local excision (WLE) with tumor free margins, however, there has been increasing evidence for the efficacy of Mohs micrographic surgery (MMS) in recent years.
-

Corpus Cavernosum Abscess Secondary to Traumatic Perforation of Urethral Diverticulum
Thomas C. Gore, Anna Schepcoff, and Domenick Sorresso
A corpus cavernosum abscess is a rare condition. Usual etiologies include penile injection of erectile dysfunction medications or illicit drugs, priapism, sexually transmitted infections, and trauma; however, there have been reported cases of idiopathic etiology. The most common causative organisms include Staphylococcus aureus, Streptococci, and Bacteroides [1]. Diagnosis is typically made clinically and through imaging (computed tomography [CT] and ultrasound). The first-line treatment is the use of intravenous (IV) antibiotics and surgical drainage. More conservative treatment, however, includes aspiration in conjunction with IV antibiotics [2-3]. Urethral diverticulum (UD) is the formation of a saccular outpouching of the urethral lumen. Symptoms may include recurrent urinary tract infections, incontinence, hematuria, and dysuria [4]. We present a unique case of a corpus cavernosum abscess secondary to perforation of a UD through self-catheterization.
-

Acral Lentiginous Melanoma: A Rare Variant with Unique Diagnostic Challenges
Taylor Gray, Brett Brazen, Maheera Farsi, and Richard Miller
Acral lentiginous melanoma (ALM), named for its location and histological growth pattern, is a rare variant of melanoma. ALM presents on palms, soles, or in association with the nail unit.1 While ALM accounts for approximately 5% of melanomas diagnosed each year, it is the most commonly diagnosed subtype of melanoma in non-Caucasian patients.
-

The Evil Twin: The Case of Heterotopic Pregnancy
Rashmi Jadhav, Vegas Brown, and Gabriel Cabrera
- Heterotopic pregnancy occurs in about 1 in 30,000 naturally conceived pregnancies (5). The risk rises 1-3% for pregnancies occurring through assisted reproductive technologies (ART) (1).
- Isolated ectopic pregnancy affects an average of 1 in every 150 live births (1).
- A known pre-existing intrauterine pregnancy (IUP) can be falsely reassuring and delay the diagnosis of a potentially life-threatening concurrent ectopic pregnancy.
- Presentation is vague and 45% of patients have no symptoms (5).
- Differential Diagnoses: endometritis, incomplete miscarriage, ruptured ovarian cyst, non-GYN cause (ie: appendicitis or UTI).
- Risk Factors: Infertility treatment, in vitro fertilization (IVF), prior ectopic, prior tubal surgery, use of IUD, smoking (1).
- These patients are more likely to have spontaneous or medically induced abortions, and are 30% less likely to have live-birth delivery.
- Laparoscopy or laparotomy are standard of care. They carry a 58-70% success rate of parturition for the IUP (1).
-
Idiopathic Chylopericardium: A Rare Entity
Seema Jaga, Joseph Namey, Christiano Caldeira, and Salah Al-Andary
- Idiopathic chylopericardiumis a rare entity in which the acculumation of chylousfluid surrounds the pericardial space.
- Herein, we present a case of a 50 year old healthy female patient with no known past medical history that was diagnosed with idiopathic chylopericardiumand was successfully treated using a pleurXcatheter drainage for two and a half weeks and a low fat diet.
-

Teriparatide and its Bone Healing Power
Aneeta J. Joseph, Jesus L. Penabad, and Antonio Pinero-Pilona
Teriparatide, a parathyroid hormone analog, is an important anabolic agent approved by the U.S. Food and Drug Administration to increase bone mineral density in osteoporotic patients. Parathyroid hormone (PTH) regulates calcium, phosphate, and active vitamin-D metabolites. The amino terminal peptide fragments of PTH has been known to increase bone mass and are being used in clinical practice for osteoporosis management.3 Teriparatide increases bone density of lumbar spine and femoral neck, and decreases the risk of vertebral and non-vertebral fractures both in postmenopausal women and men. It is also known to prevent fractures in patients with osteoporosis and promote healing of fractures.
-

Novel Infection Status Post Electrocution Requiring a 4th Ray Amputation
William R. Judson, John D. Murphy, Phillip H. Sussman, and John N. Harker
- Prevotella bivia is an anaerobic, non-pigmented, Gram-negative bacillus species that is known to inhabit the human female vaginal tract and oral flora. It is most commonly associated with endometritis and pelvic inflammatory disease.1, 2
- Rarely, P. bivia has been found in the nail bed, chest wall, intervertebral discs, and hip and knee joints.1 The bacteria has been linked to necrotizing fasciitis, osteomyelitis, or septic arthritis.3, 4
- Only 3 other reports have described P. bivia infections in the upper extremity with one patient requiring amputation2, and one with deep soft tissue infection requiring multiple debridements and extensive tenosynovectomy.5
- Delays in diagnosis are common due to P. bivia’s long incubation period and association with aerobic organisms that more commonly cause soft tissue infections leading to inappropriate antibiotic coverage.
- Here we present a case on P. bivia that resulted in extensive tenosynovectomy, multiple irrigations and debridements and eventually amputation of the 4th ray and digit of the hand.
-

Fracture Blisters
Jessica Khabra, Jinal K. Patel, Gauthier L. Stepman, Kulveer Dabb, Kenny Hernandez, Debra Angelo, and Johnathan Frunzi
Fracture blisters are tense vesicles or bullae that develop on edematous skin following some acute long bone fractures. Fracture blisters are infrequently seen, as the reported incidence is 2.9% to 6.6%.1 This rare complication, may not regularly be encountered by Physicians in the hospital. Fracture blisters typically occur within 24-48 hours following high energy trauma injuries & may last up to several weeks. Ultimately, this condition can lead to prolonged hospital stay due to an increased risk of infection and delay in surgical intervention.2 Early recognition of this dermatologic complication may be helpful in reducing hospital stays.
-

Vitamin D Deficiency and Perceived Pain
Theodore Korty, Adam Grunbaum, Ken Baxa, and Olu Oyesanmi
Vitamin D deficiency has been shown to contribute to the onset of musculoskeletal pain, headaches, and fatigue (1, 2). Deficient levels of calcium phosphate have been linked to musculoskeletal pain associated with vitamin D deficiency (3). Low levels of calcium phosphate may result in an inadequately mineralized bone matrix, and normalization of vitamin D levels should help to diminish symptoms of pain by correcting suboptimal mineralization of bone matrix (3). One prior study of patients who underwent orthopedic procedures (including treatment of vertebral compression fractures, Colle’s fractures, hip & knee arthroplasty, ligament repair, and meniscal repair), showed that 44% (n = 272) had evidence of vitamin D insufficiency (20-32 ng/mL) or deficiency (< 20 ng/mL) (4).
-

End the Glow!
Roli Kushwaha, Anthony Furiato, and Justin McNamee
Aortic dissection (AD) is part of a group of acute aortic syndromes consisting of intramural aortic hematoma, penetrating aortic ulcer, and aortic rupture. On its own, the incidence is ~3 to 8 cases per 100,000 per year, and up to 25% of cases are missed. The in-hospital mortality when treated is 27%, and with a 2% increase in mortality/hour. Imaging modalities like CT angiography, TEE, and MRA have made improved diagnosis of the disease, but are costly, potentially harmful, time consuming, and require patient stability when in use (1). The key question we have as emergency department providers is if there is a way to risk stratify patients for AD and if so, is there a test with high enough sensitivity and negative likelihood ratio (-LR) to rule out aortic dissection. Smooth muscle myosin heavy chain is a proposed modality, which is released from injured aortic media at the start of AD but there is a lack of observational studies testing its efficacy as biomarker in making the diagnosis (2). Hence, algorithms to aid physician in reducing both misdiagnosis and overtestingis much needed.
-

Evaluating Awareness of Low-Dose Computerized Tomography For Lung Cancer Screening
Roshni LeBoutillier, Bansi Savla, Vincent Wu, Zia Khan, Erick Mejia, Leah Tehranchi, My Myers, Khine Min, Jennifer Broyles, and Stacy Chase
In the U.S., excluding melanoma, lung cancer is the leading cause of cancer-related deaths.1
Cigarette smoking is the number one risk factor and is linked to 80-90% of lung cancer deaths.2
Low-dose Computerized Tomography has been shown to reduce lung cancer deaths by 20% in randomized control trials and observational studies.4
The U.S. Preventative Task Force recommends annual screening for lung cancer with low-dose computerized tomography (LDCT) in adults ages 55-80 years of age who:- Have a 30 pack-year smoking history and
- Currently smoke or
- Have quit within the past 15 years.
-

Bilateral Sporotrichoid Cutaneous Atypical Mycobacterial Infection Due to Primary Inoculation
Erin Lowe, Alexa Broderick, and Richard Miller
The group of mycobacterial species that excludes Mycobacteria tuberculosis and Mycobacteria leprae is known as nontuberculosis or atypical mycobacteria. Nearly all atypical mycobacteria species can cause cutaneous infection. The diagnosis is challenging as disease may take months to become clinically apparent, morphology is non-specific, routine culture has a low sensitivity, and organisms can be sparse on histopathologic examination. Antibiotic resistance and further complicates management. The Gulf Coast is the highest incidence region of cutaneous atypical mycobacterial infections. Here we present a challenging case of bilateral sporotrichoid atypical mycobacterial infection due to primary inoculation.
-

A Case of Systemic Sclerosis Sine Scleroderma
Adrian Lugo, Andrew Cappiello, Nemer Dabage, and Guruswamy Ramamurthy
- Scleroderma and systemic sclerosis are autoimmune phenomena that can cause progressive and permanent damage to the organs of the human body.
- They can cause fibrosis of various internal organs, including the kidneys, lungs, GI tract, and heart
- Rarely, the only manifestation of systemic sclerosis is severe hypertension with renal failure, a subset known as systemic sclerosis sine scleroderma.
-

A Rare Case of Leprosy in West Florida
Adrian Lugo, Taylor Studsrud, Nemer Dabage, and James DeMaio
- Leprosy is caused by acid-fast bacilli of the M. leprae complex, which includes M. leprae and M. lepromatosis.
- Transmission in the U.S. is rare, but has been documented in hunters who handle wild ninebanded armadillo.
- The origins of M. leprae infection among armadillos, the geographic range of the infected animals, and the potential risks infected armadillos present to people have been topics of concern.
- The infection originated amongst armadillos decades before they were ever used in leprosy research, and numerous surveys have confirmed that armadillos in the southern United States are a large natural reservoir for M. leprae; its prevalence exceeds 20% in some locales.
-

A Case of Medication-Induced Diffuse Alveolar Hemorrhage in Neurofibromatosis Type 1
Ashar Mahmood, Liz Palmer, Rebecca Schuyler, Svitlana Sharpovalova, Bilal Nadeem, Mukesh Mehta, Salman Muddassir, Nikolay Mitzov, and Monicka S. Felix
- Amiodarone, an antiarrhythmic and apixaban, an anticoagulant have been associated with diffuse alveolar hemorrhage (DAH).
- Cases have been documented demonstrating DAH in the setting of amiodarone and apixabantreatment, however there are few cases examining DAH in combination therapy.
- We present a case of diffuse alveolar hemorrhage in the setting of amiodarone and apixaban treatment for paroxysmal atrial fibrillation.
- NF1 is know to have higher risk for major bleeds due to their friable vasculature.
-

Iatrogenic Pneumothorax with Subsequent Subcutaneous Emphysema
George Michael, Eric Yuschak, and My Myers
Lung cancer is the leading cause of cancer-related death in the United States, accounting for 13% of all new cancer diagnoses and 24% of all cancer deaths.1 Transthoracic CT-guided biopsy (CTGB) is commonly used as a diagnostic tool for lung cancer, with high diagnostic accuracy, sensitivity, and specificity. 2 This procedure, however, is not without its risks which include pulmonary hemorrhage and iatrogenic pneumothorax (IPNX). Emergent chest tube placement is standard care of treatment for massive or symptomatic IPNX, commonly with the use of smaller caliber chest tubes. 2 There is, however, a growing discussion over use of larger caliber chest tubes in select patients who may pose a greater risk of developing subcutaneous emphysema (SE).5 We discuss a case of a patient with underling lung mass who underwent GTGB and developed IPNX with subsequent SE.
-

Hailey-Hailey Disease Successfully Treated with Low-Dose Naltrexone
John Moesch and Richard Miller
Hailey-Hailey disease (HHD) is an uncommon autosomal dominant disorder resulting from a mutation in the ATP2C1 gene resulting in dysfunction of the Golgi apparatus calcium-associated ATPase, thus interfering with intercellular calcium signaling.
HHD presents clinically as flaccid blisters and erosions in intertriginous areas, especially the axillae and groin.
The major histologic finding is acantholysis throughout the spinous layer of the epidermis, commonly referred to as a “dilapidated brick wall” appearance.
The initial lesions and associated symptoms usually develop during the second or third decade of life.
Complications of HHD include infections (bacterial, fungal, and viral), and malignant transformation (cutaneous squamous cell carcinoma).
-

Bilateral Posterior Fracture-Dislocation of the Proximal Humerus After First-Time Seizure
John D. Murphy, Phillip Braunlich, and Mohit Bansal
Fractures of the proximal humerus are commonly associated with osteoporosis and comprise 5.7% of all adult fractures [1]. Posterior dislocations of the shoulder comprise 2-5% of all shoulder dislocations, and when bilateral are even more infrequent, occurring less than 5%. [2,3]. Posterior dislocations are often associated with motor vehicle accidents, seizures, or electrical shock [4]. Fracture-dislocations of the proximal humerus occur in only 1% of all shoulder dislocations, thus making posterior fracture-dislocations off the proximal humerus exceedingly rare [5]. In this case report, we present a previously undescribed case presentation and treatment for bilateral posterior fracture-dislocations of the proximal humerus [7,8,9,10,11,12,13,14,15]. The purpose of sharing this case is to describe treatment options for a rarely encountered orthopedic trauma presentation, as there is currently a lack of existing medical literature.
-

Impact of Order Set Use on Stroke Care
Bilal Nadeem, Edward Waseleski, Meryem Maras-Casey, Sabih Alam, Adnan Faruqui, Michael Gutierrez, Maruthsakhi Molugu, Christina Oricompil, Ashar Mahmood, Katherine Torralba, Fatima Agha, Nour Tlimat, Olu Oyesanmi, Irina Davis, Salman Muddassir, and Nikolay Mitzov
- A case control study on stroke patients was recently completed for a quality improvement (QI) investigation.
- The objective was to determine if the use of either Hemorrhagic or Ischemic Stroke Order Set had an effect on the length of stay (LOS) or adherence to current stroke guideline recommendations
-

Impact of Order Set Use on Stroke Care
Bilal Nadeem, Edward Waseleski, Meryem Maras-Casey, Sabih Alam, Adnan Faruqui, Michael Gutierrez, Maruthsakhi Molugu, Christina Oricompil, Ashar Mahmood, Katherine Torralba, Fatima Agha, Nour Tlimat, Olu Oyesanmi, Salman Muddassir, and Nikolay Mitzov
A case control study of 118 patients from Oak Hill Hospital between the months of August 2019 and January 2020 was recently completed for a hospital research quality improvement study. The objective was to determine if the use of either Hemorrhagic or Ischemic Stroke Order Set had an effect on the length of stay (LOS) or adherence to current stroke guideline recommendations when compared to its disuse. Results indicate use of either the Hemorrhagic or Ischemic Stroke Order Set led to a decreased length of stay and an increased adherence to current stroke guideline recommendations. Limitations of the study included non-adherence to the current 2019 stroke guidelines defined by The American Stroke Association .
-

Acute Hypoxic Respiratory Failure Due To Organizing Pneumonia With Lipoid/Cholesterol Component Caused By THC Vaping With E-Cigarette
Jinal K. Patel, Kiran Tirumalasetty, Jessica Khabra, Imran Khan, and Johnathan Frunzi
Vaping has been the new and deemed “safer” way to inhale addictive chemicals such as nicotine and tetrahydrocannabinol (THC), but it does not encompass the detrimental effects of other ingredients in these vaping cartridges that can cause lung injury[1,2]. Similar studies with dabbing (heating THC wax concentrate at high temperatures with butane) showcase rapidly progressing lung injury with massive consolidation and lasting effects on lung parenchyma over a period of time [3]. This case report aims to educate people, especially the younger generation, of the dangers of newer ways of combustible alternatives that have been marketed as a “safer” way to ingest addictive compounds. Here, we report a case of a patient with THC vaping with Electric-Cigarette causing Organizing Pneumonia with Lipoid Component.
-

A Case of Pott's Disease: Typical Presentation of an Uncommon Disease in the United States
Neha Patel, Ravi Patel, Marek Krysztofiak, and K V. Sundaresh
Pott’s disease (PD), also known as tuberculosis spondylitis, is a rare disease of the spine which is typically caused by extraspinal infection. The basic lesion in Pott's disease is a combination of osteomyelitis and arthritis, usually affecting more than one vertebra. The anterior aspect of the vertebral body adjacent to the subchondral plate is commonly involved. Spinal TB can include any of the following: progressive bone destruction leading to vertebral collapse and kyphosis, cold abscess formation (due to extension of infection into adjacent ligaments and soft tissues), spinal canal narrowing by abscesses, granulation tissue or direct dural invasionresulting in spinal cord compression and neurologic deficits.(1) Although the incidence of PD has recently increased in Europe and the United States, mainly due to immigration and an epidemic of acquired immune deficiency syndrome, it is still a rare disease. Here we present a patient who immigrated from India a few months ago who presented to the emergency room with mid back pain and was found to have Pott’s disease confirmed by biopsy and PCR testing.
-

Effect of an Electronic Order Set on Newborn Hepatitis B Immunization Rates
Daniel Pedersen, Angelina Rodriguez, Michael King, and Heather Schramm
-
Internal Hernia as a Late Complication of Roux-en-Y Gastric Bypass Procedure
Samantha Purton, Gabriel Meshekow, My Myers, Edgar Mercado, and Allan Katz
As the prevalence of obesity continues to rise, so does the popularity of bariatric surgery. Previously the Roux-en-Y gastric bypass was the most common bariatric procedure, but now falls second to the gastric sleeve. It remains a relevant procedure, however, accounting for 17% of bariatric procedures in 2018. Due to its prevalence, it is important that the radiologist be familiar with the procedure and its complications such as leak, obstruction, stricture, or, as in this case, internal herniation through a mesenteric defect. Internal hernias are more commonly associated with the laparoscopic approach versus open. This is likely due to fewer adhesions created to secure the bowel, allowing more freedom for herniation and potential volvulus formation. It is imperative that the surgeon close all mesenteric defects created during the procedure to decrease the risk of this dire complication.
-
Giant Splenic Artery Pseudoaneurysm Rupture Presenting as Hemorrhagic Shock
Jaya Sanapati, Parth R. Desai, Locke W. Barber, Johnathan Frunzi, and Timothy Lee
A 56-year-old Asian male was brought to the emergency department by first responders after he developed severe, sudden-onset headache and chest pain at his home. Past medical history was insignificant. On arrival to the emergency department, the patient was in respiratory distress. Vital signs revealed temperature of 36.0°C, blood pressure of 71/44, heart rate of 90 beats per minute, respiratory rate of 18 breaths per minute, and oxygen saturation of 95% with delivery of oxygen at 2 liters per minute via nasal cannula. Examination of the abdomen revealed diffuse tenderness. Laboratory findings and arterial blood gas analysis revealed normocytic anemia (hemoglobin 7.6 mg/dL) and an anion gap metabolic acidosis with low arterial pH (7.260) and elevated lactic acid (11.0 mg/dL).
Computed Tomography (CT) of the abdomen and pelvis revealed a splenic artery pseudoaneurysm, with cross-sectional area of 5.8 x 5.6 cm, and intra-abdominal fluid collections consistent with hemoperitoneum. The patient received transfusion of packed red blood cells and resuscitation with intravenous crystalloids. He subsequently underwent selective splenic artery arteriogram and coil embolization with resolution of pseudoaneurysm filling and extravasation. The following day, exploratory laparotomy with hematoma evacuation and intra-abdominal washout was performed. The patient was given the Haemophilus influenzae type B, pneumococcal, and meningococcal vaccines and discharged.
-

Evolving de Winter Presentation of Acute Myocardial Infarction
Caroline Shepherd and Anthony Furiato
de Winter ECG pattern first detailed in 2008 in a case series Diagnostic criteria
- Tall, prominent, symmetric T waves in the precordial leads
- Upsloping ST segment depression >1mm at the J-point in the precordial leads
- Absence of ST elevation in the precordial leads
- ST segment elevation (0.5mm-1mm) in aVR
Strongly correlated with acute LAD occlusion
-
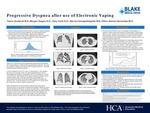
Progressive Dyspnea after use of Electronic Vaping
Taylor Studsrud, Morgan Zegers, Gary Cook, Narrani Kanapathippillai, and Hilton Alemar-Hernandez
-

A Case Of Babesiosis Seen Outside Of Its Endemic Area And Outside Of Its Incubation Period
Kiran Tirumalasetty, Jinal K. Patel, Gauthier L. Stepman, Bassem Zeidan, K V. Sundaresh, Parth R. Desai, and Johnathan Frunzi
Babesiosis Microti is a parasitic alveolate that is usually transmitted by Ixodes scapularis ticks. In the United States, the endemic areas of Babesiosis include the Northeast and Upper Midwestern regions [1]. Symptoms include fever, malaise, fatigue, vomiting, and jaundice [1]. Current therapy primarily consists of a combination of azithromycin and atovaquone. Clindamycin and quinine may be administered in severe cases. For its emerging health risk worldwide, clinicians must be aware of the several presenting manifestations of babesiosis. Since 2017, the Centers Disease Control and Prevention (CDC) has deemed Babesiosis is a reportable disease. This case focuses on the importance of recognizing Babesiosis outside of its endemic area, and that was past the average incubation period associated of 1-9+ weeks.
-

A Novel Indication for Oocyte Cryopreservation Prior to Autologous Hematopoietic Cell Transplantation for Refractory Multiple Sclerosis
Neal R. Trulock, Luke Ying, Edward Zbella, and Mark Sanchez
Multiple sclerosis (MS) is an immune mediated inflammatory diseases of the central nervous system characterized by focal ovoid like lesions of demyelination seen on MRI(1,2). The etiology of MS is unknown, however inflammation followed by CNS demyelination and axonal degeneration are known to be part of the pathologic processes that lead to the disease (1). The mean age of onset of MS is 28-31 years old and tends to affect women more often then men with a ratio of 2.3:1 (3,4) . Other risk factors associated with MS include vitamin D deficiency, smoking, and certain viruses (5). The pattern of the disease can be classified as either Relapsing or Progressive depending on whether the patient has periods with or without symptoms (6). MS is diagnosed clinically with MRI used to support the diagnosis. In cases where the diagnosis isn’t clear the McDonald diagnostic criteria can be applied (2). The life expectancy is reduced 7-14 years compared to the general population with increased deaths from infection, cardiovascular disease, respiratory disease, and suicide (7). Treatment can be divided into acute flairs, chronic, and symptomatic. The acute flairs are generally treated with steroids or plasma exchange, while the chronic disease is generally treated with disease modifying therapy (DMT)(5). No known treatment cures MS or completely prevents progression, however, which has led to many novel therapies. One of the promising therapies being explored for the past 2 decades is autologous hematopoietic cell transplants (AHCT).
-
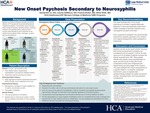
New Onset Psychosis Secondary to Neurosyphilis
Samantha Linda Jane Vu, Lauren Angela DeMarco, Francis Butler, and Nihal Shah
Syphilis is a highly contagious sexually transmitted infection (STI) caused by the spirochetal bacterium Treponema pallidum. Transmission occurs through direct contact of painless ulcerative lesions, chancres, located on the genitalia (penis, labia) and oral mucosa. Neurosyphilis is any involvement of the central nervous systems (brain, meninges, or spinal cord) by the bacterium.
-

Segmental Neurofibromatosis: Isolated Eruption of Neurofibromas on the Scapula in a Middle-Aged Man
Christopher White, Brett Brazen, and Richard Miller
-

Malignant Degeneration of Spiradenoma of the Eyebrow
Christopher White, Kristin Witfill, and Richard Miller
Spiradenocarcinoma is a malignancy of eccrine origin, with only 120 reported cases in the literature.1 Elderly males and females are equally affected.2 Benign spiradenomas along with their malignant counterpart are more frequent in patients with Brooke-Spiegler syndrome or familial eccrine spiradenoma, owing to the increased incidence of folliculosebaceous-apocrine tumors seen with these entities.3
-

A Rare Cause of Pneumoperitoneum
Robert Zusman, George Michael, Anna E. Augustin, My Myers, and Dudith Pierre-Victor
Pneumoperitoneum is most commonly associated with a perforated viscus. When free air is seen on imaging, the most common course of action is an emergent exploratory laparotomy. However, pneumoperitoneum may not always be indicative of a perforated bowel. In the case described below, we will discuss a patient who developed acute peritonitis and pneumoperitoneum after undergoing chest compressions during cardiopulmonary resuscitation (CPR) and positive pressure mechanical ventilation.
Featuring scholarly activity from HCA Healthcare Graduate Medical Education residents in the West Florida Division.
Printing is not supported at the primary Gallery Thumbnail page. Please first navigate to a specific Image before printing.

