Division
East Florida
Hospital
HCA Florida Aventura Hospital
Specialty
Emergency Medicine
Document Type
Poster
Publication Date
2023
Disciplines
Emergency Medicine | Medicine and Health Sciences | Public Health
Abstract
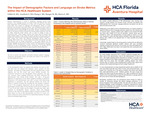
Background: Effective evaluation of stroke symptoms necessitates a comprehensive clinical assessment, influencing the timely administration of tissue plasminogen activator (tPA). This study examines the relationship between patients’ preferred language as well demographic factors and stroke care metrics within the framework of the HCA Healthcare System.
Methods: A retrospective study design was used to examine the national HCA database for all patients admitted to an HCA hospital with a diagnosis of stroke and with a recorded NIH stroke scale (NIHSS) between the years of 2017 and 2022. 37,956 patient visits from 170 HCA hospitals were analyzed to compare stroke metrics including tPA administration times (as measured from the arrival time of the patient in the emergency department (ED) to the time the tPA was administered), time to brain CT (as measured from the arrival time of the patient in the ED to the initiation time of the CT scan), NIHSS and hospital length of stay (LOS). We also evaluated whether demographic factors and language spoken affected the tPA administration rates among stroke patients.
Results: tPA administration rates were affected by sex, ethnicity, age and insurance status. Hispanics were slightly more likely to get tPA than non-hispanics (8.7% vs 7.8%, p<0.001), men were slightly more likely to get tPA than women (8.4% vs 7.7%, p=0.027) and younger aged patients were more likely to get tPA than older patients (age <45: 11.4%, 45-64: 8.9%, 65-84: 7.3%, >85: 7.5%, p<0.001). Privately insured patients were the most likely to get tPA compared to Medicaid, Medicare and uninsured patients. There was no difference in English vs non-English speaking patients and tPA administration rates. Language, sex, ethnicity, race, age and insurance status did not impact tPA administration times, however time to CT brain was impacted by age with older aged patients having a significantly shorter time to CT than younger aged patients. NIHSS was affected by age and insurance status with lower NIHSS in younger aged patients and patients with private insurance or uninsured. Additionally, the hospital LOS was significantly longer in non-English speaking patients than English speakers (7.05 days vs 6.13 days p=<0.001). Hospital LOS was also significantly longer for black patients and Medicaid patients.
Conclusions: The results of this retrospective study suggest there are differences in stroke management based on sex, ethnicity, race, age and insurance status. Most notably, men, Hispanics, younger aged patients and those with private insurance were the most likely to get tPa when presenting to the hospital with a stroke. Despite those differences, time to tPa was not impacted by any of the studied demographic factors. Language did not impact tPa administration rates, tPa administration times or the time to CT brain. Further research should be aimed to determine the reason behind these demographic differences in tPA administration rates as well as hospital LOS. Larger scale prospective studies should also be conducted to further stratify patients into specific preferred languages.
Recommended Citation
Yelkin, Henry; Goodwin, Glenn; Chang, Jonghoon; Mauger, McHenry; and Marra, Erin, "The Impact of Demographic Factors and Language on Stroke Metrics within the HCA Healthcare System" (2023). East Florida Division GME Research Day 2023. 21.
https://scholarlycommons.hcahealthcare.com/eastflorida2023/21