-
Severe Case of Systemic Lupus Erythematosus in a 36-year-old Male
Aleeza Ali, Max Kaito, Stanley Dennison, Hanan Zisling, Esam Khalifa, and John Romano
Systemic Lupus Erythematosus (SLE) is a multifactorial autoimmune disease that is capable of involving almost any organ in the body, leading to significant morbidity and mortality in affected patients. SLE is characterized by pathogenic autoantibodies that react with antigens and form immune complexes, resulting in tissue damage and a potential wide array of manifestations, including arthralgias, lupus nephritis, pleuritis, and delirium. Experts cite the effect of estrogens or factors related to the X chromosome as possible explanations regarding the increased prevalence of SLE in women over men, with ratios of up to 15:1. Here, we discuss the case of a 36-year-old male patient with a history of SLE who presented to the emergency department for worsening fatigue, nausea, and vomiting. On admission, the patient was found to have a pericardial effusion, pleural effusion, ascites, and acute renal failure. During his first day of stay at the hospital, the patient suffered a cardiac arrest, requiring endotracheal intubation, emergent pericardiocentesis, thoracentesis with drainage of 1.5 liters of pleural fluid, and paracentesis with drainage of 1.5 liters of peritoneal fluid. Interdisciplinary efforts from the ICU, IM, cardiology, pulmonology, cardiothoracic surgery, nephrology, infectious disease, neurology, IR, and pain management teams were vital in returning this patient to baseline functional status over the course of a long, complicated hospital stay. Through this case, we highlight the various, severe complications SLE is capable of inflicting upon the body, with a particular focus directed towards the rare but more critical presentation males with SLE may adopt. Additionally, we emphasize the role of public health and insurance status in the prognosis of patients with SLE, as our patient’s inability to adhere to outpatient medical therapy undoubtedly played a contributory role to his acute decompensation and near-fatal outcome.
-

Multiple Sclerosis in a 32-Year-old Female with History of Prolactinoma
Aleeza Ali, Jesse Simon, and Adekunle Bamgboye
Among disorders affecting the central nervous system (CNS), excluding trauma, multiple sclerosis (MS) is the most common cause of permanent disability in young adults. This condition is characterized by IgG autoantibody-mediated destruction of oligodendrocytes in the brain and spinal cord. Although the origin of MS is not fully understood, some suggest that prolactin may be involved in the development of the disease process evidenced by the fact that it predominately affects women of childbearing age, and the diverse role of prolactin (PRL) as a peptide hormone, cytokine, and immune modulator. Here we review the case of a 32-year-old female with history of a prolactinoma and MS presenting to HCA with an acute flare. In 2022, the patient presented to her physician with blurred vision in bilateral temporal fields, amenorrhea, and galactorrhea. She was found to have elevated serum prolactin and a 4.7 x 2 mm left lateral pituitary microadenoma on magnetic resonance imaging (MRI). She was subsequently diagnosed with a prolactinoma, and treated with cabergoline after which her symptoms resolved. Following a repeat MRI, the microadenoma from the previous year was redemonstrated, and, notably, new lesions in the periventricular white matter were discovered. Upon further work up, she was ultimately diagnosed with MS. Through this case, we may be able to better understand the involvement of PRL in the inflammatory process and triggering of autoimmune disease, such as MS.
-

Inpatient Outcomes in Patients with Cyclic Vomiting Syndrome and Cannabis Use Disorder: A Retrospective Study
Ali Tariq Alvi, Hasnan Ijaz, and Pallavi Aneja
Please see supplemental content for full abstract with tables.
Background: Cyclic vomiting syndrome (CVS) is an idiopathic disorder characterized by recurrent bouts of vomiting with intervening periods of normal health. It is commonly seen in young adults with symptoms of nausea, vomiting and dehydration. It can also lead to multiple complications including, electrolyte derangements, metabolic alkalosis, and esophageal injury. With increasing use of cannabis in United States for medicinal and recreational purposes, the impact of its use in different patient populations remains unclear. Therefore, in this study, we aimed to assess the burden and impact of cannabis use disorder (CUD) on inpatient outcomes in patients admitted with cyclic vomiting syndrome.
Methods: The Hospital Corporation of America (HCA) corporate database from 2016 to 2021 with relevant ICD-10 codes were used to identify patients with cyclic vomiting syndrome and cannabis use disorder (CUD). We compared demographics, including age and sex, and outcomes of patients with cyclic vomiting syndrome with vs without cannabis use disorder (CUD). Outcome variables were all-cause mortality, length of hospital stay, acute kidney injury (AKI), sepsis, shock, intestinal obstruction, and encephalopathy, compared between CUD vs non-CUD cohort among hospitalized patients with cyclic vomiting syndrome. Multivariate regression analysis was also performed adjusting for demographics.
Results:A total of 10179 adult patients (age 18-90) with cyclic vomiting syndrome were identified in our study, of which 2515 (24.71%) had a reported cannabis use disorder. The CUD cohort had a median age of 32.6, as compared to 33.3 in non-CUD cohort. It consisted predominantly of female patients (54.08%). Among inpatients outcomes, the CUD cohort had a higher rate of acute kidney injury (AKI) (12.52%) as compared to non-CUD cohort (2.74%) with statistical significance (p value
Conclusion: Our study showed higher rate of development of acute kidney injury and sepsis in patients with cannabis use disorder with cyclic vomiting syndrome. The development of AKI could be attributed to intravascular volume depletion by persistent vomiting and dehydration, leading to reduced renal blood flow. Cannabis use disorder can lead to increase susceptibility to certain infections, which could contribute to increased rate of sepsis in these patients. It should pave the way for conducting further observational studies in order to assess the association of renal dysfunction and sepsis with cannabis use in patients with CVS. It should also create awareness among clinicians to keep AKI and sepsis as potential complications is such patients.
-

Second Victim Syndrome: Nurturing Well-being and Resilience in the Medical Community
Daniel Basselgia
Please see supplemental content for full abstract with references.
Second Victim Syndrome (SVS), a phenomenon observed in healthcare, refers to the emotional, psychological, and physical distress experienced by healthcare providers involved in adverse patient events. This paper explores the multifaceted impact of SVS on healthcare professionals, the underlying contributing factors, and proposes comprehensive strategies to foster well-being and resilience within the medical community. By recognizing and addressing SVS, healthcare organizations can create a supportive environment that enhances the overall quality of patient care and ensures the long-term vitality of their workforce.
-

Cardiac Tamponade in the Setting of Severe Sepsis and Adrenal Insufficiency
Ayesha Choudhry, Matthew Cardeiro, Angelina Hong, and Adekunle Bamgboye
Introduction: Pericardial effusions can have various etiologies, including infectious, autoimmune, drug induced, endocrinologic, among others. Cardiac tamponade occurs when large effusions compress the heart and can lead to obstructive shock.
Case Description: A 48-year-old female with a history of hypothyroidism and pituitary adenoma resection presented with subjective fevers and generalized weakness for the past 5 days. She was lethargic with muffled heart sounds on exam. Vitals showed a heart rate 95 beats per minute, blood pressure 63/51, respiratory rate 18 breaths per minute, with normal temperature. Labs on admission were significant for white blood cell count of 11,500/L, hemoglobin 10.8 g/dL, sodium of 126 mmol/L and lactate 3.7. Electrocardiogram showed normal sinus rhythm with nonspecific ST and T wave changes. Further workup was consistent with secondary adrenal insufficiency (AI). Chest computed tomography demonstrated ground glass opacities with cephalization of the pulmonary vessels, bilateral pleural effusions and a large pericardial effusion. Transthoracic echocardiogram showed the large pericardial effusion with moderate right atrial collapse.
She underwent emergent pericardial window with drainage of 700 mL of serous dark fluid. Blood cultures were negative, and fluid culture grew Enterococcus faecalis. She received empiric antibiotics on admission, as well as intravenous fluids and parenteral hydrocortisone with subsequent stabilization of blood pressure and electrolyte abnormalities.
Discussion: This is a unique case of cardiac tamponade in a patient who had adrenal insufficiency and suspected sepsis on admission. Cardiac tamponade can mimic septic shock, and early recognition of it is critical, as treatment is emergent pericardiocentesis. A few case reports have documented this peculiar association between AI and cardiac tamponade, and AI is hypothesized to increase the risk of small or moderate pericardial effusions progressing to life threatening tamponade.
-

A Case of Transient Left Bundle Branch Block
Taylor Craig, Vincent Grekoski, Kashan Mahmood, and Laura Tortora
Please see supplemental content for full abstract with references.
Episodic bundle branch blocks are a phenomenon associated with many clinical conditions seen in the emergency department. Intermittent BBBs by definition show both normal conduction and BBB within a single electrocardiographic tracing, where a transient BBB is described as a conduction defect that which then returns to normal. The most common cause of both transient and episodic BBB is rate related however there are many causes.1 Acute LBBB should lead to suspicion of acute coronary syndrome until proven otherwise, however other many other precipitating causes can factor into the overall clinical picture.
-
Surviving the Apprehensive Methicillin-Sensitive Staphylococcus aureus (MSSA) Bacteremia: A Case of Bacteremia with an Undetermined Source of Infection Leading to Suspected Cardioembolic Ischemia and Biochemical Septic Shock
Greisy D. Curbelo Sesin, Eduardo Marino-Urbino, Christopher Fontela, Melanio J. Rodriguez, Jorge A. Diaz, Shivaan C. Oomrigar, Ramon Mendoza Bello, and Yoandy Rodriguez Fuentes
Introduction: This research presents a complex case of a 70-year-old male with acute metabolic encephalopathy and biochemical septic shock, later attributed to cardioembolic ischemia, resulting from Methicillin-Sensitive Staphylococcus Aureus (MSSA) bacteremia with an elusive source of infection.
Case Description: The 70-year-old patient, with a medical history of hypertension and aortic valve stenosis status post-Coronary Artery Bypass Grafting and bioprosthetic valve replacement on dual anti-platelet therapy (clopidogrel and aspirin), was admitted following an unwitnessed fall and a day of vomiting and generalized weakness. Upon arrival, the patient exhibited altered mental status, hypotension, and acidosis. Initial diagnostic workup raised suspicion of biochemical septic shock and a possible postictal state. Upon arrival to the Emergency Department, patient was seen by trauma services for (+) HS, (+) LOC, (+) AP. Patient underwent a PAN-SCAN that showed no acute intracranial hemorrhage or mass effect, no acute post traumatic intrathoracic process, no acute post-traumatic abdominopelvic process nor post-traumatic thoracic or lumbar spine injury. Pelvis X-ray showed no evidence of acute fracture or dislocation. Lab-work was remarkable for acute metabolic acidosis, initial K was 2.35, bicarb 8, lactic acid 4.4, calcium 4.0 and Mag 1.1. Subsequent brain MRI revealed cardioembolic ischemia and subarachnoid hemorrhage concurrent with MSSA bacteremia. A multidisciplinary approach involving ICU, neurology, interventional cardiology, and infectious disease specialists ensued, leading to comprehensive evaluations, including transesophageal echocardiography and MRI of the spine. Despite an exhaustive workup, the source of infection remained elusive. Treatment encompassed fluid resuscitation, corticosteroids, broad-spectrum antibiotics, and antiviral therapy.
Discussion: This case underscores the intricate challenges in managing a patient with biochemical septic shock, cardioembolic ischemia, and MSSA bacteremia without an identified source of infection. Such cases are exceedingly rare, with an incidence of less than 1%. The multidisciplinary approach was instrumental in facilitating a successful outcome, resulting in the patient's complete recovery from the initial encephalopathic state. The study highlights the importance of collaborative care to mitigate the high mortality and poor prognosis associated with similar cases of undetermined MSSA bacteremia.
-
Persistent Challenges: Pulmonary Hypertension in Aortic Coarctation Despite Surgical Valve Replacement
Adam Devine and Jacklyn Garcia
Introduction: Aortic coarctation has an incidence of 0.04% and is typically amendable either through a surgical or interventional approach. Unfortunately, patients that have undergone repair of the coarctation are at risk of systemic hypertension which suggests a more diffuse vasculopathy. The arteriopathy can also affect the pulmonary vasculature leading to pulmonary hypertension (PH). The development of PH is a poor prognostic factor. Patients with a history of coarctation repairs have more significant afterload measurements which stiffen their left ventricle and decrease compliance and diastolic function. Adults with Coarctation of the aorta (CoA) are at increased risk of premature cardiovascular death or heart failure secondary to persistent subendocardial fibrosis. We present a case of pulmonary hypertension in a patient with CoA status post surgical aortic valve replacement (SAVR).
Case Presentation: Our patient is a 35 years old female with a history of PFO, ASD, HTN, subclavian stenosis, and CoA who presented with 6 months of worsening dyspnea. The patient underwent SAVR with bioprosthesis twice. Workup included a chest x-ray denoting cardiomegaly and pleural effusions. A new 6/6 systolic murmur was discovered on exam. CTA chest displayed a 4.7 cm ascending aorta with multiple saccular aneurysms. 2D echocardiogram was significant for moderate to severe AS, no TR, and normal PAP. Her workup was positive for hemolytic anemia suggestive of blood vessel vs cardiac valve related hemolytic anemia requiring transfusion. An elective cardiac catheterization was performed due to persistent dyspnea and was positive for severe PH with a PCWP 44 mmHg. The patient was referred to CT surgery for further evaluation for a redo SAVR.
Conclusion: Our case emphasizes the complexities involved in managing CoA and mitigating the development of pulmonary hypertension in spite of SAVR. The underlying pathophysiology linking CoA and PH and its risk of increased mortality warrants further investigation.
-
Subacute Stroke Like Presentation Likely due to Disseminated Histoplasmosis in an Immunocompromised Patient
Ashley R. Diaz, Priya Mohan, Utmitha Konda, Alfonso Manotas, and Issac Ichoa
Histoplasmosis capsulatum is an opportunistic fungal infection that is largely asymptomatic and found to have nonspecific signs and symptoms. It predominates in Central and North America, and is one of the leading causes of hospitalization among the fungal family. However, in the right host, such as in this case, a patient with significant immunosuppression can develop serious manifestations as it disseminates outside of the pulmonary system. The challenging element of disseminated histoplasmosis is that despite proper treatment immunocompromised patients will frequently relapse with worsening presentation. There is limited literature on subacute stroke-like presentation in a patient with chronic infection of histoplasmosis, yet this patient has been repeatedly admitted over the last 10 months and found to show significant improvement upon receiving antifungal treatment. We hereby present a case about a young female patient in her late 20’s with a past medical history of congenital HIV, and hydrocephalus status post a ventriculoperitoneal (VP) shunt that presented to the emergency department with left sided weakness of the upper and lower extremities, dysarthria, and left facial droop. On brain imaging, some subacute MCA ischemia involving the right frontal, parietal, and basal ganglia and worsening cerebritis was found. The patient also underwent a lumbar puncture showing leukocytosis, and hyperproteinorrachia. Despite inconclusive findings in the CSF the patient was treated with amphotericin B intravenously and her mental status and motor deficits improved almost instantly.
-

Examining Nationwide Disparities in Managing Critical Limb Threatening Ischemia among Individuals with Diabetes Mellitus or End-Stage Kidney Disease by Race and Ethnicity
Daniel Dominguez and Waseem Wahood
Please see supplemental content for full abstract with tables.
Introduction: Critical Limb Threatening Ischemia (CLTI) presents a significant challenge, particularly for individuals with diabetes mellitus (DM) or End-Stage Kidney Disease (ESKD). Healthcare disparities related to race and ethnicity are a pressing concern. This study aims to examine a 16-year trend to assess whether the disparities in managing critical limb-threatening ischemia (CLTI) are diminishing among individuals with diabetes mellitus (DM) or End-Stage Kidney Disease (ESKD).
Methods: The analysis involved an examination of the National Inpatient Sample data from 2005 to 2020, with a focus on hospitalizations related to CLI. Identification of the types of revascularization procedures performed and the presence of comorbidities, specifically DM and ESKD, was conducted. To investigate disparities, the utilization of these procedures among different racial groups, including White, Black, Hispanic, Asian and Pacific Islander (AAPI), Native American, and Others, was compared. Hierarchical, multivariable regression models were employed, adjusted for patient and hospital demographics, as well as the Elixhauser Comorbidity Index Score, to evaluate race-related differences in procedure utilization and major amputations.
Results: Among the 5,762,426 admissions involving DM and CLTI patients, 64% were White. In comparison to White patients, Black DM patients exhibited a 0.22% higher trend in revascularization utilization (p<0.001), while Hispanic DM patients showed a 0.24% higher trend (p<0.001). Major amputation utilization was 0.21% lower for Black DM patients (p<0.001) and 0.13% lower for Hispanic DM patients (p<0.001), with AAPI patients also experiencing a 0.23% lower trend (p<0.001). All racial groups had higher odds of receiving revascularization and major amputations. Among 856,188 admissions involving ESKD and CLTI patients, 46% were White. In comparison to White patients, Black DM patients exhibited a 0.14% higher trend in major amputation utilization (p=0.023), and Hispanic DM patients showed a 0.27% higher trend (p=0.001). Conversely, for ESKD, Black patients exhibited a 0.26% lower trend in major amputation utilization (p<0.001), Hispanic patients a 0.13% lower trend (p=0.030), and AAPI patients a 0.37% lower trend (p=0.005). All racial groups, except Native Americans, had higher odds of receiving revascularization and major amputations.
Conclusion: This analysis has provided compelling evidence of enduring disparities in the treatment of CLTI among patients with DM or ESKD within our nationally representative sample. A notable pattern emerged, with all racial groups, except White patients, demonstrating a higher likelihood of undergoing both major amputations and revascularization procedures for CLTI. These results highlight not only the persistence of healthcare disparities but also the critical need for more targeted and equitable approaches in managing CLTI, especially when patients contend with concurrent comorbidities. The interpretation of these findings points to the urgency of addressing disparities in CLTI treatment. It suggests that factors beyond clinical necessity may be influencing treatment decisions and access to interventions. Further investigation is warranted to explore the root causes of these disparities, potentially encompassing healthcare access, socioeconomic factors, and cultural considerations. By comprehensively understanding these dynamics, healthcare systems can tailor interventions to ensure that all patients, regardless of their racial or ethnic background, receive timely and appropriate CLTI care, ultimately striving for improved patient outcomes and healthcare equity.
-

Late Onset Sheehan Syndrome 23 Years After Post-Partum Hemorrhage
Igbayilola Dosunmu, Ali Tariq Alvi, Sarah Kaufman, and Ayesha Malik
Please see supplemental content for full abstract with figures and references.
Sheehan syndrome is defined as ischemic necrosis of pituitary gland following massive postpartum hemorrhage leading to panhypopituitarism. It has an insidious course with multitude of presentations. The majority of cases remain undiagnosed for many years after the delivery with average time following postpartum hemorrhage to diagnosis of Sheehan syndrome is believed to be almost 13 years according to one study. Here, we present a unique case of late onset of Sheehan syndrome 23 years after the last childbirth which was complicated by hemorrhage. To our knowledge, this is the second reported case of onset of disease after more than 20 years.
-

Burkholderia cepacia Causing ARDS in a Patient Without Cystic Fibrosis
Igbayilola Dosunmu, Shahriar Sharif, Samyukta Swaminath, Nashit Mozumder, and Diego Marin
No abstract available.
-

Massive Small Bowel Resection in a 74-year-old Patient with Atrial Fibrillation-Induced Mesenteric Ischemia
Armand Edalati, Bita C. Behaeddin, Raul Aguilar, and Shaikh Hai
Acute mesenteric ischemia (AMI) in the setting of atrial fibrillation is a life-threatening abdominal emergency that requires immediate localization and clinical intervention to restore mesenteric perfusion for the prevention of developing bowel necrosis. As bowel ischemia rapidly progresses, serum metabolic derangements become prominent, guiding practitioners on effective therapeutic options. Ultimately, mesenteric ischemia progressively bolsters the possibility of a patient developing multiple organ dysfunction. Due to this minacious pathogenesis, rapid time to diagnosis can become the difference between life and death. Intraoperatively, emergent surgical intervention regarding bowel resection needs to be thoroughly reviewed and planned based on the patient's medical history and overall prognosis. Excessive bowel resection can consequently lead to the development of short bowel syndrome, a complex life-altering disease that manifests as chronic nutritional deficiency, steatorrhea, and failure to thrive.
We present a case of a 74-year-old African American female with a past medical history significant for atrial fibrillation (managed with the generic drug Rivaroxaban). The patient was transferred to Westside hospital from Baptist Urgent Care with complaints of acute abdominal pain. An abdominal computed tomography (CT) scan revealed a closedloop obstruction, prompting emergent surgical intervention after administration of K-centra as a Rivaroxaban reversal agent. Intraoperatively, 210cm of small bowel was resected due to observed irreversible ischemic changes. Mesenteric thrombosis with resultant large-segment small bowel resection was established to be the postoperative diagnosis.
This case emphasizes the importance of considering mesenteric thrombosis as a potential etiology in patients presenting with severe abdominal pain and a history of atrial fibrillation. Prompt recognition and intervention, including surgical resection, in conjunction with appropriate blood product replacement and antifibrinolytic therapy, can significantly contribute to favorable patient outcomes. Further studies are warranted to explore optimal management strategies and long-term prognosis in similar cases.
-

Where’s ADAM? Successful Treatment of COVID-19 Vaccine-Related Refractory Thrombotic Thrombocytopenic Purpura
Christopher Fontela, Alfredo Toll, Jose Fernandez, Gabriel Barciela-Perez, Jorge Diaz, Greisy Curbelo-Sesin, Ilde Manuel Lee, and Jose Gascon
A 54-year-old man with a medical history notable for hypertension and type 2 diabetes mellitus presented with altered mental status. Initial assessment revealed altered consciousness, aphasia, and diffuse generalized petechiae. Having recently migrated from Colombia, he had received four doses of the Pfizer COVID-19 vaccine, with the last dose administered one month prior to presentation. Laboratory results indicated severe thrombocytopenia (platelet count: 3), microangiopathic hemolytic anemia, acute myocardial, liver, and kidney injury, prompting a presumptive diagnosis of thrombotic thrombocytopenic purpura (TTP). Confirmation was achieved through an ADAMTS13 level of less than 2 percent. Despite initiating high-dose solumedrol and emergent plasmapheresis, the patient's neurological status deteriorated six days into treatment, necessitating mechanical ventilation, suggestive of treatment resistance, confirmed by persistent ADAMTS13 levels under 2 percent. In addition to high-dose steroids and daily plasmapheresis, Rituximab was introduced due to poor prognosis and refractoriness. Remarkably, Caplacizumab, a Von Willebrand factor-directed monoclonal antibody, was initiated alongside the aforementioned treatments, resulting in notable clinical improvement. The patient's neurological status fully recovered, along with resolution of end organ damage, underscoring the potential of Caplacizumab in treating refractory thrombotic thrombocytopenic purpura induced by COVID-19 vaccination or the virus itself.
This case underscores the emergence of acquired refractory TTP due to COVID-19 vaccination or viral exposure, emphasizing the significance of early identification through comprehensive vaccination history and titers. Furthermore, the successful application of Caplacizumab highlights its efficacy in managing refractory thrombotic thrombocytopenic purpura.
-

Invasive Testing for Pre-operative Localization of Parathyroid Tumors
Akua Graf, Craig Cochran, Samira Sadowski, Naris Nilubol, William F. Simonds, Lee S. Weinstein, Richard Chang, and Smita Jha
Context: The identification of parathyroid tumor(s) in patients with persistent/recurrent primary hyperparathyroidism (PHPT) is critical for a successful re-operative surgery. If non-invasive studies (ultrasound, CT, MRI, sestamibi) fail to conclusively localize the tumor, invasive procedures (arteriography and selective venous sampling) are performed.
Objective: To describe our experience with invasive studies for parathyroid tumor localization and provide follow-up data on selective arterial hypocalcemic stimulation with central venous sampling, a technique developed at our center.
Methods: We identified patients who underwent preoperative invasive testing for localization of parathyroid tumor from 1991-2020. The result of each invasive localization study (arteriogram, hypocalcemic stimulation and selective venous sampling [SVS]) was categorized as true-positive (TP), false-positive (FP) and false-negative (FN) based on histology and biochemical outcome.
Results: 94 patients with 96 tumor occurrences underwent invasive testing for parathyroid tumor localization. Arteriogram, hypocalcemic stimulation and SVS accurately localized the tumor in 47 of 94 (50%), 56 of 93 (60%) and 51 of 62 (82%) tumors, respectively. Hypocalcemic stimulation was more likely to correctly localize the tumor when arteriogram showed a blush (37 of 50 (74%) vs. 19 of 43 (44%), p = 0.01). When both arteriogram and hypocalcemic stimulation yielded concordant positive findings, SVS did not change management in the 18 cases in which all three were performed. Twelve patients remained with persistent PHPT, all had recurrent disease with multiple affected glands.
Conclusions: Hypocalcemic stimulation is a useful adjunct in patients with PHPT who require invasive localization and can obviate the need for SVS.
-

Acute Multiorgan Failure in a 27-Year-Old Non-Drug User
Tatiana Gusan, Angelina Hong, Sarah Kaufman, and Nathan Zaher
Introduction: Hypertensive emergency is defined as a systolic blood pressure greater than 180 mmHg or diastolic pressure over 120 mmHg with signs of end organ damage. The pathophysiology of a hypertensive emergency leads to an inability to maintain tissue perfusion resulting in organ hypoxia that often leads to temporary, and in more severe cases, permanent damage.
Case Description: A 27-year-old gentleman with no known past medical history presented with acute bilateral blurry vision, headache and bilateral lower extremity weakness for the past two days. His blood pressure was 266/169 and heart rate 99 beats per minute on presentation. Bloodwork demonstrated a creatinine level of 6.3 mg/dL, blood urea nitrogen 50 mg/dL, troponin I 0.466 ng/mL, hemoglobin 9.3 g/dL, platelet count 92,000/uL, low haptoglobin and elevated LDH levels. His platelet count was previously within normal limits. Schistocytes were noted on blood smear. His magnetic resonance imaging of the brain showed a 3 mm punctate acute ischemic infarct in the right parietal lobe. He was started on a nicardipine drip and transitioned to oral antihypertensives the following day. Renal function stabilized and he did not require renal replacement therapy. He was discharged on aspirin and a statin, as well as a blood pressure regimen of metoprolol tartrate, hydralazine, and nifedipine.
Discussion: This was a rare presentation of a young male with no past medical history who presented with microangiopathic hemolytic anemia and acute renal failure secondary to a hypertensive emergency. It stood out as the laboratory abnormalities were indicative of microthrombi formation in the systemic vasculature as a result of endothelial damage, similar to more commonly described pathologies such as TTP and HUS.
-

Save a Limb: Potential Utility of Empiric Plasmapheresis for Recurrent Brachial Artery Thrombosis and Acute Limb Ischemia following Left Heart Catheterization
Peter Harrill, Mariel Duchow, and Levy Amar
Please see supplemental content for abstract with figures.
Background: Although radial artery thrombosis following left-sided cardiac catheterization is a recognized complication, with an incidence reported anywhere from 1-10%, there are very few reports of recurrent brachial artery thrombosis and acute limb ischemia following such a procedure.
Case: 64-year-old female with past medical history of a previous CVA of unknown etiology with no residual deficits and hyperlipidemia who was initially admitted for management of a suspected NSTEMI. She was started on an IV Heparin infusion prior to undergoing a Left Heart Catheterization, which was normal, using right radial artery access. Within the next 24 hours, the patient developed ipsilateral brachial, radial, and ulnar artery thrombi, identified initially via ultrasound and confirmed intraoperatively. She was urgently taken to the operating room where a thrombectomy and angioplasty were performed. Unfortunately, these isolated thrombi continued to reoccur in her brachial, radial, and ulnar arteries despite adjustments in anticoagulation which had included a switch to argatroban as well as several intra-operative boluses of argatroban. Her ACT and aPTT remained persistently subtherapeutic. She underwent surgical thrombectomies over 4 consecutive days with removal of the recurrent thrombi.
Decision-Making: Hematology was consulted and labs were sent to work-up possible antiphospholipid or anticardiolipin syndrome in addition to vasculitis. Given concerns for these processes and the patient’s critical condition at the time, a shared-decision was made to trial plasmapheresis. She was continued on argatroban and dual anti-platelet therapy was initiated as well. Ultimately, the patient required a total of six operations, including the initial left heart catheterization as well as a subsequent fasciotomy performed emergently for acute compartment syndrome. Following all of the aforementioned medical and surgical management, including a total 5-day course of empiric plasmapheresis, the patient slowly began to regain sensation and strength within her right hand, although not to her previous baseline, with the aid of Physical and Occupational Therapy. She was discharged on oral forms of argatroban and dual anti-platelet therapy with her limb intact following a total of 29 days in the hospital. Laboratory work-up for the aforementioned hematologic and autoimmune entities were all negative.
Discussion and Conclusions: Prompt recognition of Acute Limb Ischemia as well as coordinated evaluation, management, and intervention from multiple medical specialties can be limb-and-life-saving. While there was not a confirmed diagnosis of any specific underlying vasculitis or autoimmune process in this instance, empiric treatment with plasmapheresis did seem to have played a positive role in the patient’s recovery; although, it would be difficult accurately quantify its effectiveness relative to all of the interventions she received. Overall, further research into the pathophysiology of the development of arterial thrombi in the setting of recent vascular manipulation is needed to further guide management of these types of cases.
-

Outcomes of Patients with COPD during the COVID Pandemic
Jacob Hentges and Julia Fashner
A scoping review of COVID-19's impact on healthcare delivery and health outcomes found disruptions in care delivery and a shift towards telemedicine(1). Another study found no significant change in the length of stay for patients admitted to the hospital for COPD exacerbation during the pandemic period compared to the pre-pandemic period(2).
We conducted a secondary analysis of HCA Florida St. Lucie Hospital data to compare the outcomes of patients with COPD before (Jan 2018 – Feb 2020) and during the COVID-19 pandemic (March 2020 – Dec 2021). The data included patients aged over 18 years who were diagnosed with COPD and did not have COVID-19 or dementia. We analyzed length of stay (LOS), ICU admission, and mortality on a monthly basis for the two time periods using chi-square and Fisher’s exact tests.
There was no significant difference in ICU admissions or mortality between the two time periods. The LOS did not differ for most months, except for statistically significant differences in January, June, and November (p<0.05). These months coincided with spikes in COVID-19 hospitalizations during 2020 and 2021, which may have impacted resources for caring for COPD patients and contributed to longer LOS.
Our secondary analysis suggests that the COVID-19 pandemic may have had an indirect impact on LOS for patients with COPD, but not on ICU admission or mortality. However, further research is needed to fully understand the factors contributing to these trends.
1. Roy CM, Bollman EB, Carson LM, Northrop AJ, Jackson EF, Moresky RT. Assessing the indirect effects of COVID-19 on healthcare delivery, utilization and health outcomes: a scoping review. Eur J Public Health. 2021 Jul 13;31(3):634-640. doi: 10.1093/eurpub/ckab047. PMID: 33755130; PMCID: PMC8083627.
2. Poucineau J, Delory T, Lapidus N, Hejblum G, Chouaïd C, Le Coeur S, Khlat M. Hospital admissions and mortality for acute exacerbations of COPD during the COVID-19 pandemic: A nationwide study in France. Front Med (Lausanne). 2022 Sep 16;9:995016. doi: 10.3389/fmed.2022.995016. PMID: 36186789; PMCID: PMC9522972.
3. Jennifer Y. So, Nathan N. O'Hara, Blaine Kenaa, John G. Williams, Christopher L. deBorja, Julia F. Slejko, Zafar Zafari, Michael Sokolow, Paul Zimand, Meagan Deming, Jason Marx, Andrew N. Pollak, Robert M. Reed, Population Decline in COPD Admissions During the COVID-19 Pandemic Associated with Lower Burden of Community Respiratory Viral Infections, The American Journal of Medicine, Volume 134, Issue 10, 2021, Pages 1252-1259.e3, ISSN 0002-9343, https://doi.org/10.1016/j.amjmed.2021.05.008.
-

The Re-Emergence of an Ancient Disease: A Case Presentation of Spinal Tuberculosis
Danay Herrera, Nargisa Ergasheva, Paola Solari, Daniel Kaswan, and Bryan Greendield
Please see supplemental content for full abstract with references.
Introduction: An ancient disease identified in Egyptian and Peruvian mummies, tuberculous spondylitis caused by Mycobacterium tuberculosis (MTB) is considered the most common form of extrapulmonary tuberculosis (TB) [1,5]. Despite the identification of the causative agent, the improvement in diagnostic tools, the production of the Bacillus Calmette-Guerin (BCG) vaccine, and the development of antimicrobial regimens since the disease was first described, it remains a major health burden today with significant morbidity and mortality among developing countries [5]. Spinal TB can lead to severe deformity and permanent neurological deficits, as such early recognition and hastened treatment are necessary to prevent irreversible damage [1,2]. Here we describe the case of a 24-year-old immigrant male who presented with worsening back pain found to have spinal TB confirmed through PCR testing.
-

Atraumatic Splenic Rupture: An Unaccustomed Complication of H. parainfluenzae Endocarditis
Daniel P. High, Jose M. Acosta-Rullan, Danay Herrera, and Mauricio Danckers
No abstract available.
-

Post-procedural Vertebroplasty/Kyphoplasty Outcomes of Patients from 2010-2020
Issac Ichoa, Waseem Wahood, Shyam Kurian, Mohamad Bydon, Jonathan Morris, David F. Kallmes, and Waleed Brinjikji
Introduction: Vertebroplasty/kyphoplasty are common procedures used to treat vertebral compression fractures. The most common precipitating factor is osteoporosis, although there are other causes such as trauma, spinal tumors, etc. These procedures utilize fluoroscopy by inserting a trocar into the pathological vertebra. Once the trocar is in place, bone cement is then inserted into the vertebra in a vertebroplasty to help stabilize the fracture. In a kyphoplasty, a balloon is inserted after the trocar and is slowly inflated to correct the collapsed vertebra before injecting the cement. These procedures are commonly performed in an outpatient setting and generally yield good outcomes with minimal complications. However, in this study we take a deeper dive into the post-procedural outcomes of vertebroplasty/kyphoplasty.
Methods: In this cohort study, we collected and analyzed data from the National Surgical Quality Improvement Project (NSQIP) to follow the post-procedural outcomes of 4,145 patients who underwent vertebroplasty/kyphoplasty for 11 years (2010-2020). The number and type of complications, as well as reoperations from 2011-2020 (4,117 patients), were trended to assess post-procedural outcomes. Complications include: surgical site infection, wound disruption, pneumonia, unplanned intubation, pulmonary embolism, renal insufficiency, renal failure, ventilation, urinary tract infection, myocardial infarction, deep vein thrombosis, sepsis, septic shock, and return to the operating room. The year 2010 was not used in these trends due to small sample size.
Results:From 2011-2020, there was an uptrend of +0.27% per year in the proportion of reoperations (p=0.036). Simultaneously, there was an uptrend of +1.11% per year in the proportion of any complication due to vertebroplasty/kyphoplasty (p
Conclusion: Our analysis demonstrates the increase of reoperations and complications following vertebroplasty/kyphoplasty from 2011-2020. These outcomes may be useful for future procedures by helping drive more detailed pre-procedural screenings, follow-up care, and staff readiness of possible peri-operative complications.
-

A Case of Hyperkalemia Secondary to Table Salt Alternative in a Patient with Normal Renal Function
Souhil M. Jaafil, Laura Tortora, Erin Marra, and Steven Shapiro
Introduction: Hyperkalemia is a commonly presenting electrolyte derangement, usually secondary to chronic kidney disease or medication use. In one retrospective study by Singer et al of 100,260 Emergency Department (ED) patient visits it was found that 1 in 11 ED patients presented with a potassium derangement (1). Patients can present in various ways, from asymptomatic to life threatening arrhythmias. A less commonly recognized cause of hyperkalemia is dietary substitutions for everyday table salt. Ayach et al reported a patient with potassium of 9.8 mmol/L secondar to dietary substitutions but with acute kidney injury and ACE inhibitor use (2). Through a detailed literature review, we found that it is uncommon for patients to present with hyperkalemia with normal renal function and predisposing medications to hyperkalemia. The case we are presenting is that of a patient with normal kidney function, and no other known risk factors for hyperkalemia, presenting with an initial potassium of 9.0 mmol/L after the initiation of common table salt replacement.
Case Presentation: A 60-year-old female with no reported medical history presented to the emergency department for generalized weakness, nausea and 1 episode of emesis onset today, with diarrhea that started 3 days prior. During the evaluation in the ED, an EKG, chest x-ray, labs (CBC, CMP, Troponin, pro-BNP, Lipase, TSH w/ reflex T4, Urinalysis) were ordered. Initial CBC was un-remarkable, while initial CMP was significant for a hyperkalemia at 9.0 mmol/L with sodium at 133 mmol/L and creatinine of 0.70 mg/dL. A re-draw was immediately ordered and confirmed a potassium level of 8.9 mmol/L. All other lab draws were un-remarkable. EKG was significant for peaked T waves, with normal QRScomplexes. The patient was treated for hyperkalemia with 3 grams of calcium gluconate, 10mg of nebulized albuterol and 5 units Insulin with 25 mL of D50W. The intensive care team was consulted, and the patient was admitted to the intensive care unit for close monitoring of her potassium levels. The patient’s final potassium level upon discharge was 3.5 mmol/L Upon discussion with the patient of her lab results showing hyperkalemia, the patient revealed that she had recently started a table salt replacement called Nu-Salt because her primary care physician advised her to decrease her sodium intake. Nu-Salt is a popular salt substitute that if formulated with potassium chloride rather than sodium chloride. As there was no history of kidney disease, no evidence of acute kidney injury, or history of medication use linked to hyperkalemia, we attributed the use of large amounts of Nu-Salt to this patient’s acute hyperkalemia.
Discussion: Our case report demonstrates the importance of obtaining a thorough history, including recent changes to their diet, as well as the need to educate our patients on proper nutrition substitutions.
References:
- Singer AJ, Thode HC Jr, Peacock WF. A retrospective study of emergency department potassium disturbances: severity, treatment, and outcomes. Clin Exp Emerg Med. 2017 Jun 30;4(2):73-79. doi: 10.15441/ceem.16.194. PMID: 28717776; PMCID: PMC5511959.
- Ayach T, Nappo RW, Paugh-Miller JL, Ross EA. Life-threatening hyperkalemia in a patient with normal renal function. Clin Kidney J. 2014 Feb;7(1):49-52. doi: 10.1093/ckj/sft151. Epub 2013 Dec 30. PMID: 25859350; PMCID: PMC4389164.
-

A Case of Coxsackievirus Type B-Induced Myocarditis Presenting with GI Symptoms
Daniel Karpel, Jason Nguyen, Cristina Benites, Mohammed Akram, Francini Alcocer-Guzman, Evelyn Garcia, Shany Quevedo, Ambar Sekulits, and Livasky Concepcion Perez
Please see supplemental content for full abstract with references.
Myocarditis affects 1.5 million people worldwide and in chronic forms can lead to heart failure. This inflammatory disorder is a primary cause of dilated cardiomyopathy globally and is frequently a complication of viral infections. Although Coxsackievirus B3 continues to be a prominent causative agent, further exploration has discovered a number of Coxsackie serotypes responsible for myocarditis. Despite being a well-known contributor to congestive heart failure, there is a lack of conventional techniques available to aid in diagnosis, making diagnosing acute viral myocarditis a complex and tedious process. We discuss the case of a 25 year old woman presenting with acute viral myocarditis complicated with gastroenteritis and congestive hepatopathy. This case highlights the ways in which the virus can manifest itself and emphasizes the importance of early clinical suspicion, diagnosis, and management.
-
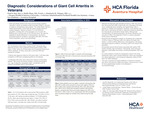
Diagnostic Considerations of Giant Cell Arteritis in Veterans
Paul Kay, Molly Phan, and Kimberly M. Winges
Please see supplemental content for full abstract with references.
Introduction: Giant cell arteritis (GCA) is the most common primary systemic vasculitis in adults, but studies to date have been limited in volume or subject to retrospective meta-analysis.1 The United States Veterans Health Administration (VHA) holds the nation’s largest electronic medical database. Veterans comprise 7% of the American population, including 24% of the population over 75 years old.2 Building upon a clinical study of one VHA site cohort,3 we used this database to identify differences in demographics, risk factors, associated systemic conditions, and biopsy yield within the entire veteran population using novel methodology.
Methods: This retrospective cohort study included 24,857 individuals with codes for GCA or temporal artery biopsy (TAB) since 1/1/2001 within the VA Informatics and Computing Infrastructure (VINCI) database. Patients with diagnosis codes for GCA given within 14-60 days after completion of TAB were considered positive for the disease. Unadjusted odds ratios were used as the measure of association between TAB results and clinical variables, including demographic (e.g., age at diagnosis, geographic region, and gender) and 18 medical comorbidities seen in GCA patients.
Results: Of 10,470 patients with a documented TAB procedure, 2285 were positive (21.8%). Mean age at diagnosis was 72.9 (95% CI [72.5, 73.3]) years, with highest prevalence between 70-79 (828 patients, 36.4%). Mean age at diagnosis was higher in males (73.2, 95% CI [72.8-73.6]) versus females (68.1 [66.3-69.9]), and odds of positive TAB were higher in males than females (OR 1.26 [1.04-1.52]). Odds of GCA were higher in patients with polymyalgia rheumatica (OR 2.05 [1.82-2.31]), aortic aneurysm dissection (OR 1.17 [1.02-1.34]), and amaurosis fugax (OR 1.12 [0.96-1.31]).
Conclusion: Our findings identify several clinical factors associated with positive and negative TAB results within the VHA and is the largest study to date on this disease.
-

Residency Burnout and Wellness
Harmanjit Khokhar and Dennis Cardriche
Intro: Wellness and burnout are two components of residency. Burnout is defined as a condition defined by emotional exhaustion, depersonalization, and decreased feelings of accomplishments. Wellness is the accumulation of positive habits affecting mental, physical and emotional health. Burnout has been associated with “negative effects on quality of care, patient satisfaction and patient safety (1).”
The Objective: Objective of this review is to explore the connection between wellness and burnout, as well as future considerations, including research. While further research on burnout is an important avenue to pursue, tangible interventions may shed light on protective factors against the negative effects of burnout. A major barrier for research is measurable outcomes regarding burnout and wellness because there is a distinct lack of parameters that are used universally. This highlights the significance of creating tangible outcomes. Burnout and wellbeing are interconnected, creating interventions that target both aspects of residency training will help increase self-efficacy and create positive, lasting habits residents can utilize further into their careers.
The Methods: The review articles selected for further investigation, ranging from being published between 2015-2019, include Residency Wellness: An Intervention to Decrease Burnout and Increase Resilience and Happiness (1); Optimizing Resident Education and Wellness through the Learning Environment (2) and Evidence-Based Interventions that promote Resident wellness from the Council of Emergency Residency Directors (3). Article selection was based on inclusion of burnout and wellness as factors in residency, ways to explore how factors in the environment may affect these factors and evidence-based techniques to help safeguard individuals in residency who may be vulnerable. Review article 1 presents small measurable interventions that help residents recognize burnout, wellness and provides them with tools to help mitigate burnout. Review article 2 dissects the contributing factors that may negatively affect residents and make them prone to burnout, as well present tangible suggestions for each factor. Review article 3 focuses on Emergency Medicine residency specifically, and also provokes the question of how residency burnout and wellness can be defined across all medical specialities.
Discussion: In review article 1, residents selected for this intervention may be more open to including these interventions and may not necessarily be applicable to all residents. In review article 2, interventions, definitions and research related to burnout and wellness is to be done under the umbrella of ACGME, when training in each specialty is inherently different from one another, making universal measures difficult to achieve. In review article 3, focuses only on the speciality of Emergency Medicine, with research that includes other specialties. Each article cohesively addresses important factors, about defining burnout and wellness in residency, contributing factors and evidence-based interventions. Burnout and wellness is notoriously difficult to quantify, however, this should not halt research into interventions that can safeguard residents, as both topics are known to affect residency. Interventions should be conducted at an individual, program and institutional level, possibly by speciality and through experienced physicians who specialize in these topics or by specialized psychologists with training in understanding burnout and wellness in the medical field. Another aspect to be implemented is through resident feedback, with actionable measures, perhaps by each year, to be implemented the following year.
-

Risk Factors for Depression Progression in Parkinson's Disease: A Retrospective Cohort Study
David Kosoy, James Cassuto, and Gregory Kurgansky
Introduction: Depression is a common non-motor symptom in Parkinson's disease (PD) with a significant impact on quality of life and overall prognosis. Despite the availability of effective treatments, many PD patients with depression do not receive timely diagnosis and appropriate intervention. This study aimed to identify risk factors for depression progression in PD to inform clinical practice and future research.
Methods: We conducted a retrospective cohort study of PD patients using registry data from the Parkinson's Progression Markers Initiative (PPMI) dataset. The primary outcome was depression progression, defined as a 2-point or greater increase in the MDS-UPRDS depression score within the first two years of study enrollment.
Results: A total of 485 PD patients were included in the study, of which 78 (16.1%) experienced depression progression. Significant predictors of depression progression included older age at diagnosis (p=0.088), higher MDS-UPRDS Part 2 scores (motor function in activities of daily living, p=0.053), and race, with Black and Asian individuals demonstrating an over 7-fold and 4-fold increased risk, respectively, compared to White individuals (p=0.001).
Discussion: Our findings highlight the importance of depression as a risk factor for progression in PD, emphasizing the need for proactive screening and interventions targeting mental health in PD management. The identification of age, motor impairment, and race as predictors of depression progression underscores the importance of tailored approaches that address the unique needs of diverse patient populations. Further research and collaborative efforts are warranted to elucidate the underlying mechanisms, evaluate the impact of racial disparities, and develop strategies to improve outcomes and quality of life for individuals living with PD.
Conclusion: This study provides valuable insights into the risk factors for depression progression in PD, with important implications for clinical practice and future research. Additionally, our findings highlight the need for proactive screening and interventions targeting mental health in PD management, tailored to the unique needs of diverse patient populations.
-

Comparing 30-Day Outcomes of Open Versus Endovascular Revascularization for Chronic Limb-Threatening Ischemia
David Kosoy and Waseem Wahood
Abstract: Chronic limb-threatening ischemia (CLTI) is a serious condition that can lead to amputation and even death. Open and endovascular revascularization are two common treatment options for CLTI, but the optimal treatment approach remains controversial. This study compared the 30-Day outcomes of open and endovascular revascularization using data from the National Surgical Quality Improvement Program (NSQIP) database. The study included 6,780 patients who underwent open bypass with saphenous vein, 4,201 patients who underwent open bypass with alternative conduit, and 8,887 patients who underwent endovascular intervention. Compared to open bypass with saphenous vein, endovascular intervention was associated with a higher rate of major amputation (1.4% vs. 1.0%, p=0.002) and major adverse limb events (MALE, 2.8% vs. 2.1%, p=0.004). However, endovascular intervention was also associated with a lower rate of major adverse cardiovascular events (MACE, 1.6% vs. 3.5%, p<0.001). Compared to open bypass with alternative conduit, endovascular intervention was associated with a similar rate of major amputation (1.4% vs. 1.2%, p=0.763), MALE (2.8% vs. 2.2%, p=0.34), and MACE (1.6% vs. 3.3%, p=0.053). These findings suggest that endovascular intervention may be a safe and effective treatment option for CLTI, but it is important to carefully select patients who are likely to benefit from this approach. Patients with complex lesions or severe comorbidities may be better candidates for open bypass surgery.
Conclusion: This study provides valuable insights into the 30-Day outcomes of open versus endovascular revascularization for CLTI. The findings suggest that endovascular intervention may be a safe and effective treatment option for selected patients, but careful patient selection is essential.
-

Outcome Disparity Among African Americans Following Colon Trauma
Joseph Krocker, Victoria Lord, Tamar Walker, Tammy Luan, Luis Rivera Aguasvivas, Jonathan Meizoso, Heidi Bahna, and Juliet Ray
Introduction: African Americans (AA) are more likely to experience violence-related trauma compared to White subjects and experience poorer outcomes in many facets of traumatic injury. However, previous analysis of males with penetrating colon trauma has identified no difference in mortality and decreased morbidity in AAs compared to Whites. Outcomes in AAs following colon injury requiring surgery are assessed in the current study.
Methods: The Trauma Quality Improvement Program (TQIP) was queried for subjects requiring colon surgery within 24 hours of admission from 2017-2019. Mortality was the primary outcome and secondary outcomes included intensive care unit (ICU) days, total length of hospital stay (LOS) and ostomy creation. Multiple regression controlling for demographics and injury characteristics was utilized for outcome evaluation.
Results:10,899 patients selected (3,940 AA). AAs were more likely to experience penetrating trauma compared to other races (82% vs 43%; P =
Discussion: AAs experience longer ICU and hospital stays following traumatic colon injury requiring surgery. This finding is consistent with reports of disparate outcomes for AAs across a variety of trauma metrics and the driving factors warrant further exploration.
-

Unsuspected Large B-cell Lymphoma Diagnosed by Pleural Effusion Cytology after Chest Wall Trauma
Matthew Lee and Susana Ferra
No abstract available.
-

Forum Discussion Indicates Favorable Views of JAK Inhibitors for Atopic Dermatitis
Nicole Levin, Karan Rajalingam, Ashley Wentworth, and Leila Tolaymat
Background: There is increasing discussion online concerning the management of atopic dermatitis (AD). Patients often document their subjective experience of a given treatment. It remains to be determined if the experiences vary based on treatment or align with efficacy.
Objective: To determine which treatments are associated with positive or negative experiences.
Methods: The largest online AD platform was searched for posts that only discussed a singular treatment. The discovered 28,159 posts were rated “positive” or “negative” by DistilBERT, a pre-trained sentiment analysis model that derives from BookCorpus, a collection of 11,038 books containing 74 million sentences. Positive sentiment proportions (PSP), calculated as the ratio of positive posts to total posts were tabulated.
Results: The most positively rated treatments were upadacitinib (.365 CI:[.255, .475]), topical ruxolitinib (.324 CI:[.236, .412]), and phototherapy (.281 CI:[.257, .306]) (Figure 1). Conversely, the least positively rated treatments were Class V Steroids (.116 CI:[.051, .180]), Class VI Steroids (.128 CI:[.079, .178]), and Class VII Steroids (.158 CI:[.145, .171]).
Limitations: Generalizability is limited given the existence of other forums and the demographics of forum users.
Conclusion: JAK inhibitors were the most positively reviewed treatments, likely influenced by novelty and perceptions of better safety and efficacy, whereas steroids comprised the least positively rated treatments, potentially due to concern for long-term side effects.
-

Sudden Onset AMS, Focal Weakness, Fever and Aphasia due to Intracranial Subdural Empyema in Left Temporo-Parietal Lobe
Lily Hyunjung Lim, Menachem M. Nagar, and Pallavi Aneja
Intracranial subdural empyema (ISE) is a rare infection of brain, which occurs when pus is collectively located in the space between dura and arachnoid matter. In the past, its mortality was nearly 100%, if it was not treated appropriately within 24-48 hours. Thanks to improvement of diagnostic modalities and treatment, its mortality has dramatically decreased. Though, it can still cause a devastating consequence if it is not managed in a timely manner. The common etiology of ISE is different depending on the age group. In younger patients, it occurs frequently as a complication of infection in neighboring structures like sinusitis or otitis. On the other hand, in older patients, neurosurgical procedures are mostly related to ISE even though the incidence is low. Clinical presentation is similar regardless of etiologies, and it is more related to an anatomic region. Based on the clinical presentation and findings on imaging studies if suspicion for ISE is high, broad-spectrum antibiotic therapy must be initiated immediately. Most cases need surgical evacuation as well. We present a 76-year-old male who had a recent history of complication-free craniectomy due to a benign tumor and a month later developed AMS, fever, unilateral weakness and aphasia secondary to ISE in the left temporo-parietal lobe.
-

From Pest Control to Poison Control: A Novel Case Report of Delayed Carbamate Poisoning.
Kashan Mahmood, Erin Marra, Taylor Craig, and Gaurav Patel
Introduction: Carbamates are a class of insecticides structurally and mechanistically similar to organophosphate (OP) insecticides. Carbamates are N-methyl carbamates derived from a carbamic acid and cause carbamylation of acetylcholinesterase at neuronal synapses and neuromuscular junctions. While they possess a similar mechanism of action to the irreversible phosphorylation of acetylcholinesterase by organophosphates, carbamates bind to acetylcholinesterase reversibly. Subsequently, carbamates typically have a similar toxicological presentation to OP poisonings with a duration of toxicity that is typically less than 24 hours.
Case Presentation: We present a case of a 51-year-old male who was complaining of diarrhea, lacrimation, salivation, headache, photophobia, diaphoresis, and chest tightness that had progressively gotten worse over the course of 2 weeks. Two weeks prior to coming into the emergency department (ED), the patient and his wife were cleaning their home with an insecticide spray. Both the patient and his wife had symptoms that started within 24 hours of using the insecticide spray, however, the wife’s symptoms subsided after 2 days of supportive care and symptomatic treatment at the hospital. The patient’s symptoms, however, progressively worsened over the course of 2 weeks since the exposure. In the ED the patient presented bradycardic and hypotensive. His physical exam was remarkable for miosis, photophobia, diaphoresis and abdominal pain and he was in moderate distress. He was given Atropine sulfate for his bradycardia per poison control’s recommendation, ketorolac for pain, ondansetron for nausea, famotidine for reflux as well as some gastrointestinal discomfort, and sodium lactate for fluid resuscitation. His initial labs were significant for leukocytosis, elevated creatinine, lactic acidosis and hypercalcemia. Once stabilized in the ED, the patient was admitted to the intensive care unit (ICU) for close observation on telemetry and symptom control. On reevaluation before sending the patient to the ICU the patient’s status was improving from the atropine, fluids and symptom control. Once transferred to the ICU the patient was given Loperamide for his diarrhea and Atropine boluses as needed for bradycardia. Pralidoxime would have also been considered if there were any signs of muscle weakness or symptoms related to nicotinic receptor activation. Frequent neuro checks and echocardiograms were done on a scheduled basis. With supportive care and time, the patient’s clinical condition started to improve over the course of 3 days. On day 3, the patient was discharged and stayed at a friend’s home as the patient’s home needed professional cleaning.
Discussion: This case illustrates the importance of persistent signs and symptoms of a carbamate toxicity which classically subside within 96 hours after exposure. However, carbamate toxicity cannot be ruled out in someone who presents with all the classic signs and symptoms, which can persist and even progressively worsen over the course of days to weeks.
-
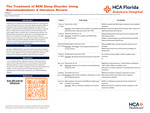
The Treatment of REM Sleep Disorder Using Neuromodulation: A Literature Review
Aaron Marbin, Shane Ragland, Orestes Hadjistamoulou, Clara Alvarez Villalba, and Samuel Neuhut
No abstract available.
-

The Treatment of Depression in Alzheimer's Disease Using Neuromodulation: A Literature Review
Aaron Marbn, Shane Ragland, Thalia Adrian, Clara Alvarez Villalba, and Samuel Neuhut
Please see supplemental content for full abstract with references.
INTRODUCTION: An estimated 44 million individuals live with Alzheimer's Dementia globally, a number expected to triple by 2050.1 Depression is a commonly observed comorbidity in individuals with Alzheimer's disease. Traditional antidepressant medications often pose challenges due to their side effects and limited efficacy in this population. As a result, alternative therapeutic approaches are being explored, with Transcranial Magnetic Stimulation (TMS) emerging as a promising intervention for treating depression in Alzheimer's patients. TMS is a non-invasive brain stimulation technique that utilizes magnetic fields to modulate neural activity in targeted brain regions without the systemic side effects associated with pharmacological interventions. We evaluated the current literature on the potential of TMS as a treatment modality for depression in Alzheimer's patients.
METHODS: A search in PubMed yielded thirteen results in English for which the full text was available. Criteria for exclusion included lack of relevance to the research question, case studies, commentaries or letters to the editor, and guideline articles. We included five studies in this review. Two independent reviewers assessed the studies.
DISCUSSION: Most of the current literature assesses the efficacy of TMS in improving cognitive function and memory while acknowledging the difficulty in discerning whether the positive outcomes seen are a sign of improved markers of AD or the commonly seen comorbid depression in this patient population. The scarcity of available literature highlights the necessity of more robust clinical studies exploring the treatment of depression in the geriatric population with comorbid Alzheimer's dementia.
-

Race/Ethnicity and Morbidity/Mortality in Laparoscopic Cholecystectomy: 2016 USA Study
Victorien Meray and Rupa Seetharamaiah
Background: Social determinants of health, such as race and ethnicity, can have a significant impact on people's health and well-being. People of color are more likely to experience poverty, lack of access to healthcare, and discrimination, which can lead to worse health outcomes. Laparoscopic cholecystectomy is a surgical procedure to remove the gallbladder. It is the most common gastrointestinal surgery performed in the United States. In this study, we sought to determine if there is an association between race/ethnicity and morbidity/mortality in adult patients undergoing laparoscopic cholecystectomy.
Methods: We conducted a non-concurrent cohort study of patients over 18 years old who underwent laparoscopic cholecystectomy at an American College of Surgeons' National Surgical Quality Improvement Program hospital in 2016. The main exposure variables were race (Black/African American, white, or other) and ethnicity (Hispanic vs. non-Hispanic). The main outcome was the probability of morbidity and mortality. Morbidity refers to any complication that occurs as a result of the surgery, such as infection, bleeding, or pneumonia. Mortality refers to death. Unadjusted and adjusted logistic regression analysis were used to calculate odds ratios (ORs) and 95% confidence intervals (CIs).
Results: Hispanics and Black/African Americans had decreased odds of mortality compared to white patients (OR 0.48; 95% CI 0.44-0.52 and OR 0.85; 95% CI 0.78-0.92, respectively). However, Black/African Americans had increased odds of morbidity compared to white patients (OR 1.43; 95% CI 1.32-1.54).
Conclusion: Social determinants of health, such as race and ethnicity, have a significant impact on patients' access to and quality of care. These factors can evolve over time, and their impact on patient outcomes is complex and multifaceted. We recommend that the American College of Surgeons (ACS) consider adding race and ethnicity to their surgery risk calculator, as our study suggests that these factors play a role in the probability of morbidity and mortality. We also encourage future studies to assess other social determinants of health, such as socioeconomic status, for inclusion in such calculators. In addition to race and ethnicity, our incidental findings suggest that length of surgery and transfer sites may also play a role in patients' probability of morbidity and mortality. Further research is needed to explore these relationships in more detail.
-

Cannabis Consumption and the Emergence of Giant Lung Bullae: A Case Report and Clinical Analysis
Rafael Miret, Jose Rodriguez Castro, Armando Cabrera, Mauricio Danckers, Raiko Diaz, and Nikhil Bhardwaj
Please see supplemental content for full abstract with figures and references.
Introduction: Vanishing Lung Syndrome (VLS), also known as idiopathic giant bullous emphysema, is a rare pulmonary condition characterized by the development of large, thin-walled bullae within the lung parenchyma. While the exact etiology of VLS remains unclear, there is growing interest in exploring a potential association between VLS and cannabis use. This case report aims to contribute to the existing body of knowledge by presenting a case of VLS in a patient with a history of chronic cannabis consumption in prior years.
Clinical Presentation: A 44-year-old former smoker male with a history of mild intermittent asthma and marijuana use presented to the hospital with concerns of shortness of breath and a non productive cough. Patient reports symptoms started one day prior to presentation and were associated with subjective fevers, chills, wheezing, and pleuritic chest pain. The dyspnea was described as constant, on rest, exacerbated by exertion, and partially relieved with albuterol inhaler. Physical exam was significant for wheezing in bilateral lung fields and decreased breathing sounds in upper lobes. A computed tomography of the chest with contrast showed bilateral massive bullae in the upper 40% of the right lung and slightly larger size in the left lung (Figure 1,2).
Pulmonary function tests at rest, performed after hospital discharge, were significant for a decreased FEV1/FVC ratio and normal DLCO consistent with asthma disorder. Alpha antitrypsin levels were within normal limits as well as autoimmune workup. Patient was referred to the cardiothoracic surgeon who intraoperatively found a giant bulla approximately 15 cm involving the anterior segment and compressing the remaining of the left lung, with significant adhesions to the pericardium, and a 10 cm bulla involving the apical portion of the posterior apical segment. As a result, it was performed a segmentectomy of a portion of the apical posterior lobe, an anterior lobe segmentectomy, lysis of the adhesions, and excision of the bulla from the superior segment. Bullous emphysema was confirmed histologically, in addition to mild chronic inflammation, vascular congestion, and focal organizing pneumonia-like features. Patient was discharged home without need for home oxygen and symptoms improvement.
Discussion: VLS is a rare lung condition which typically affects young male smokers. Bullous emphysema refers to emphysematous lung with bullae, which are air-filled spaces within the parenchyma that are 1 cm or larger in diameter and consist of a thin wall of visceral pleura with remnants of alveolar and interlobular septa inside.(1) The most common associated risk factor to developing this condition is cigarette smoking. While the exact pathophysiological mechanisms are unclear, several hypotheses have been proposed. Cannabis smoke contains various harmful compounds, including carcinogens and irritants, which could potentially contribute to the development of bullae in susceptible individuals. The radiological criterion for the diagnosis of VLS is the presence of giant bullae in one or both the upper lobes of the lung, which occupy more than one-third of the hemithorax and compresses the surrounding lung tissue (3). Significant progressive reduction of spirometry indications and reduced exercise tolerance accompanied with dyspnea are characteristic to patients with VLS. Surgical treatment is possible and effectively reduces dyspneic symptoms and significantly lowers the risk of spontaneous pneumothorax in patients with VLS. (4)
Conclusions: VATS bullectomy represents an effective therapeutic option, allowing re-expansion of compressed lung tissue and complete resolution of symptoms. It is necessary to raise awareness of this condition and discuss the similarity of bullous emphysema and pneumothorax in clinical presentation and radiographic findings, as well as the differences in treatment options.
-
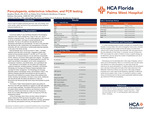
Pancytopenia, enterovirus infection, and PCR testing
Stephen Mock, Salome Herzstein, and Andrea Horbey
Introduction: This is a case of a patient presenting with fever, rash, and vomiting. Upon further studies, patient was found to have pancytopenia which started an extensive hospital work up.
Case Description: A previously healthy 9- year-old female presented to the emergency department with 3 days of tactile fever, 2 days of rash, and 1 day of nonbilious nonbloody emesis. The rash initially appeared on the trunk and by the day of admission, had begun to spread peripherally to the extremities. The rash on the abdomen was described as mild, generalized, blanchable and maculopapular. The rash on the extremities was described as mild, nonblanching, and maculopapular on the lower extremities with mild, erythematous, nonblanchable petechiae bilaterally on the soles of the hands and feet. Initial labs in the ED showed a complete blood count significant for anemia, leukopenia, thrombocytopenia, bandemia, and an ANC of 2847. Complete metabolic panel and uric acid were within normal limits. There was, however, an elevated lactate dehydrogenase and c-reactive protein. Coagulation studies were ordered and demonstrated elevated PT and INR, but PTT was within normal limits. UA showed proteinuria, but was otherwise unremarkable. COVID, Influenza, and Group A Strep swabs were negative. The patient was given Ibuprofen, Ondansetron, and Diphenhydramine in the ED. The patient was admitted to the pediatric unit for further management of pancytopenia, bandemia, acute febrile illness, and a generalized rash.
Upon admission to the pediatric unit, the patient was initially given supportive treatments, including probiotics, Famotidine, and Ibuprofen. Hematology and Oncology and Infectious Disease Specialists were consulted for further management. The Hematology and Oncology Specialist ordered a hematologic workup, which demonstrated a positive Von Willebrand Antigen of 218%, but Fibrinogen, Factor VII, Factor VIII, Factor XIII, and Von Willebrand factor ristocetin cofactor were all within normal limits. The Infectious Diseases Specialist recommended we start the patient on Doxycycline as empiric therapy while awaiting further results, including a full respiratory viral panel. The results demonstrated the patient was positive for Enterovirus and CMV IgG antibodies but negative but CMV IgM antibodies and antinuclear antibodies. Patient continued to be febrile 2 days post admission, which led us to start the patient on Ceftriaxone per Infection Disease recommendation. In due course, Ceftriaxone was discontinued after the patient was afebrile for 2 days and Doxycycline was discontinued after blood culture demonstrated no growth for 3 days. By time of discharge, blood, throat, and stool cultures indicated no growth. Strep screen, Influenza, and SARS-COV-2 NAA were all negative. Upon day of discharge, the patient was afebrile and stable with no emesis, generalized rash improving, pancytopenia improving, and appropriate PO intake.
Discussion: Pancytopenia can be associated with a wide range of diseases, some of which can be life-threatening. While it is a commonly known fact that certain viral infections can cause pancytopenia, our case study shows that enterovirus can cause pancytopenia. If a patient presents with pancytopenia and a rash that involves palms and soles of feet, keep enterovirus in the differential. Enterovirus infection can also have a wide range of disease processes and in some cases be life-threatening, especially if it affects the central nervous system, heart, or liver. It is important to perform a careful history and physical exam as well as acquire appropriate additional studies and consultations. None of the authors have any financial interests, relationships or affiliations relevant to the subject of this manuscript. This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
-

MIS Calcaneal Fracture Repair: A Literature Review
Nehal Modha, Roshni Patel, and Warren Windram
Minimally invasive surgery (MIS) has gained prominence as a viable approach for the management of calcaneal fractures, offering the potential for reduced soft tissue trauma, enhanced visualization, and expedited recovery. This literature review aims to comprehensively analyze the existing body of research on MIS techniques employed in the repair of calcaneal fractures.
A comprehensive literature review was completed by the authors using Google Scholar, Pubmed, Cochrane Review, and Science Direct using a combination of phrases related to the title of this article that focused on MIS interventions for calcaneal fractures. The review encompassed studies from the last decade, evaluating surgical techniques, clinical outcomes, radiographic assessments, and complications associated with MIS approaches.
The analyzed literature revealed a diverse array of MIS techniques, including percutaneous fixation, arthroscopic-assisted reduction, and minimally invasive plating. These techniques aimed to achieve anatomical reduction, preserve the subtalar joint, and minimize the risk of soft tissue complications often associated with open surgical methods.
Clinical outcomes demonstrated varying degrees of success, with some studies reporting improved functional outcomes and reduced wound-related issues following MIS interventions. However, the literature also highlighted the challenges posed by fracture complexity, surgeon expertise, and the potential for limited visibility in certain cases.
Complications associated with MIS approaches included hardware irritation, malreduction, and postoperative pain, underscoring the need for precise technique execution and thorough patient selection.
In conclusion, MIS techniques for calcaneal fracture repair present a promising avenue in modern orthopedic practice, offering potential advantages in terms of reduced soft tissue trauma and enhanced recovery. However, challenges remain in achieving consistent outcomes across varying fracture patterns and patient populations. Future research endeavors should aim to establish standardized protocols, refine surgical techniques, and conduct comparative studies to ascertain the true benefits and limitations of MIS approaches in calcaneal fracture management.
-

Optimal Fixation Requirements for Lapidus Bunionectomies: A Comprehensive Review and Analysis
Nehal Modha, Diego Peralta, and Warren Windram
The Lapidus bunionectomy procedure, aimed at correcting hallux valgus deformities, involves realignment of the first metatarsal-cuneiform joint and often necessitates fixation to ensure proper alignment and stability during the healing process. A comprehensive literature review was completed by the authors using Google Scholar, Pubmed, Cochrane Review, and Science Direct using a combination of phrases related to the title of this article to determine the optimal fixation requirements for successful outcomes in Lapidus bunionectomies.
A systematic search of electronic databases that reported on fixation techniques, outcomes, and complications associated with Lapidus bunionectomies. Analysis of these studies revealed a wide range of fixation methods, including staples, screws, plates, and combinations thereof. Postoperative outcomes were assessed based on radiographic alignment, functional recovery, and complication rates.
The findings suggest that the choice of fixation for Lapidus bunionectomies should be tailored to individual patient factors, including age, bone quality, and concurrent medical conditions. Screw fixation emerged as a commonly utilized method, providing stable fixation and satisfactory outcomes across various studies. Additionally, the optimal degree of fixation required remains a subject of debate. Some studies indicated that single screw fixation provided comparable outcomes to double screw fixation, while others favored the use of multiple screws for enhanced stability. Literature indicated that the most stable construct was the plate and screw construct which also allowed for early weight bearing and range of motion.
Complications associated with excessive fixation were also noted, including hardware irritation, prominent hardware, and delayed healing. Conversely, inadequate fixation was associated with postoperative malalignment and reduced stability. Achieving the balance between sufficient fixation for stability and avoiding over-fixation for reduced complications remains crucial.
In conclusion, the optimal amount of fixation for Lapidus bunionectomies remains a nuanced decision that depends on patient-specific factors. Surgeons must tailor their fixation strategies to the individual's anatomical and clinical profile, recognizing that a personalized approach offers the best opportunity for favorable outcomes. Literature indicates that plate and screw construct is the most optimal fixation construct.
-

Current Treatment Options for AVN (Freiberg's Infraction) of the Second Metatarsophalangeal Joint
Nehal Modha, Fahad Rahman, and Warren Windram
Avascular necrosis (AVN) of the second metatarsal is a debilitating condition characterized by the loss of blood supply to the bone, leading to cellular death and potential collapse of the affected metatarsal head. This study presents a comprehensive review of contemporary literature to elucidate the spectrum of treatment options available for managing AVN of the second metatarsal.
A systematic search of reputable medical databases yielded a total of 38 pertinent studies detailing various treatment modalities for AVN of the second metatarsal. The review encompassed surgical and non-surgical approaches, evaluating their efficacy, long-term outcomes, and complications.
Non-surgical interventions, such as protected weight-bearing, orthotic devices, and immobilization, have been employed to alleviate symptoms and potentially slow disease progression in early-stage AVN cases. However, these methods are often limited by the advanced nature of the condition at the time of diagnosis.
Surgical interventions offer a spectrum of options tailored to disease severity and patient factors. Core decompression, vascularized bone grafting, and metatarsal head resection have been considered in cases where conservative measures prove ineffective. Advanced techniques like osteochondral autograft transplantation and regenerative therapies hold promise for restoring articular surfaces and mitigating longterm joint dysfunction.
The choice of treatment modality is contingent upon factors including disease stage, patient age, activity level, and joint integrity. Emerging trends emphasize individualized treatment plans that consider the potential for joint preservation and pain relief.
Complications, such as joint stiffness, malalignment, and persistent pain, highlight the importance of careful patient selection and meticulous surgical technique in achieving optimal outcomes.
In conclusion, the management of AVN of the second metatarsal necessitates a thorough understanding of the available treatment options. While non-surgical interventions may be suitable for early cases, surgical interventions offer tailored solutions for advanced disease stages. Patient-specific characteristics should guide treatment decisions, with an emphasis on achieving pain relief, preserving joint function, and mitigating long-term complications. Prospective comparative studies evaluating the long-term outcomes of diverse treatment strategies are imperative to establish evidence-based guidelines for addressing AVN of the second metatarsal effectively.
-

Current Concepts of Treatment for Foot and Ankle Arthritis
Nehal Modha and Warren Windram
Foot and ankle arthritis is a prevalent and debilitating musculoskeletal condition that significantly impairs the quality of life for millions of individuals worldwide. This scientific abstract provides an overview of the current concepts of treatment for foot and ankle arthritis, highlighting the multifaceted approach employed by healthcare professionals to alleviate pain, improve function, and enhance the overall well-being of affected patients.
This comprehensive review outlines the key elements of contemporary foot and ankle arthritis management. First, it discusses the importance of early diagnosis and classification of the condition, emphasizing the role of advanced imaging modalities and clinical assessments in establishing a precise diagnosis. Accurate classification is crucial as it informs subsequent treatment decisions and helps in predicting disease progression.
The abstract then explores the non-pharmacological interventions that form the cornerstone of conservative management in foot and ankle arthritis. These include patient education, lifestyle modifications, physical therapy, orthotic devices, and assistive aids. The integration of these strategies helps mitigate pain, improve joint function, and delay disease progression.
Next, the abstract delves into pharmacological interventions, highlighting the efficacy and safety of various medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and biologic agents. The selection of pharmacological agents is based on the disease subtype, severity, and individual patient characteristics.
Surgical interventions are then discussed, encompassing a range of procedures from arthroscopy and joint-preserving surgeries to joint fusion and total joint replacement. The abstract provides insights into the indications, outcomes, and potential complications associated with surgical interventions, underscoring the importance of shared decision-making between the patient and the surgical team.
Furthermore, the abstract explores emerging therapies and technologies, such as regenerative medicine, minimally invasive techniques, and patient-specific implants, which hold promise for improving treatment outcomes in foot and ankle arthritis.
In conclusion, this scientific abstract offers a comprehensive overview of the current concepts of treatment in foot and ankle arthritis. It underscores the importance of a multidisciplinary approach, personalized care, and the integration of conservative and surgical interventions to optimize patient outcomes. As our understanding of the condition continues to evolve and innovative therapies emerge, the management of foot and ankle arthritis is poised to provide improved relief and restoration of function for those affected.
-

Plantar Plate Injury: Current Treatment Options
Nehal Modha and Warren Windram
Plantar plate injuries have gained recognition as a common cause of forefoot pain and instability. This review aims to comprehensively analyze the present landscape of treatment options available for addressing plantar plate injuries.
A comprehensive literature review was completed by the authors using Google Scholar, Pubmed, Cochrane Review, and Science Direct using a combination of phrases related to the title of this article that discussed various treatment modalities for plantar plate injuries. The review encompassed both non-surgical and surgical interventions, assessing their efficacy, outcomes, and potential complications.
Conservative approaches, such as rest, taping, orthotic devices, and physical therapy, have been employed to manage milder cases of plantar plate injuries. These methods aim to alleviate pain, correct biomechanical abnormalities, and facilitate tissue healing. However, the effectiveness of conservative measures is influenced by the severity of the injury and patient compliance.
Surgical interventions offer a range of techniques based on injury severity and patient factors. Plantar plate repair, reconstruction, and augmentation have emerged as effective strategies to restore stability and alleviate pain. Advancements in surgical techniques, including minimally invasive procedures and arthroscopic guidance, aim to improve outcomes while minimizing morbidity.
The reviewed literature emphasizes the importance of accurate diagnosis, classification, and staging of plantar plate injuries to guide appropriate treatment selection. Individualized patient assessment, including factors such as foot biomechanics, patient age, and activity level, are crucial in tailoring treatment approaches.
Complications associated with surgical interventions encompass stiffness, hardware irritation, and recurrent deformities. Thus, meticulous surgical planning, precise technique execution, and postoperative rehabilitation protocols are imperative to optimize outcomes.
In conclusion, the management of plantar plate injuries demands a nuanced understanding of the available treatment modalities. Tailored approaches, based on injury severity and patient characteristics, are pivotal in achieving successful outcomes. The treatment options are often patient specific, however anchors have shown to be superior.
-
A Case of Phlegmasia Cerulea Dolens
Stefanie Navarrete
Introduction: This is the case of a patient presenting with phlegmasia cerulea dolens after recent travel with concurrent extensive pulmonary emboli. Patient’s symptoms progressed quickly, atypically, and he did not have known common risk factor for the extent of his disease.
Case Description: The patient is a 78-year-old Caucasian male who presented to the emergency department complaining of left leg swelling and mild pain that began 1 day prior. Patient flew in 3 weeks prior from Scotland. On exam, patient was found to have extensive erythema and ecchymosis of left leg. On admission, venous ultrasound showed complete extensive thrombosis of left lower extremity extending into common femoral, greater saphenous, superficial femoral, popliteal, and into visualized calf veins. CT Chest and abdomen pelvis showed thrombosis extended up into inferior vena cava and patient had extensive bilateral pulmonary emboli. Patient was started on heparin and scheduled for thrombectomy following morning. Overnight patient’s pain progressed until thrombectomy and angioplasty was performed. Patient was discharged on anticoagulation within two days with complete resolution of symptoms.
Discussion: This patient’s case demonstrates the importance of prompt treatment in Phlegmasia cerulea dolens as the rate of amputation is 20-50%. This patient’s risk factor of immobility due to travel is a less common risk factor for this complication of DVT and his symptoms did not correlate with the extent of the disease.
-

A Young Case of Giant Cell Arteritis
Tricia O'Brien, Philip Mesquita, and Zahid Chaudhry
Introduction: Giant Cell Arteritis is condition that commonly affects patients between the ages of 70 and 80 years old. It rarely affects those younger than 50 years of age.
Description: A 40-year-old African American woman, who had previously been diagnosed with Giant Cell Arthritis via temporal artery biopsy at age 33, presented to the emergency department due to facial and arm numbness and throbbing headache. Her ESR was markedly elevated and she was placed on prednisone.
Discussion: The incidence of Giant Cell Arthritis is between 5.8 to 31.3 per 100,000 in the population. This disease affects women 2-3 times more often than men. With the average age of disease onset being age 72, this patient was particularly unique in the extremely young age of her original diagnosis. Proper diagnosis of this disease is extremely important as improper treatment can result in loss of vision.
Conclusion: This report aims to bring greater awareness to Giant Cell Arteritis in the differential diagnoses of headache in young to middle age women.
-

Microscopic Extraovarian Sex Cord Proliferations
Tricia O'Brien, Cameron Summers-Powell, and Susana Ferra
No abstract available.
-

The Location and Incidence of Neuromas as related to Metatarsal Juxtaposition on Radiographs: a Prospective Review of consecutively enrolled patients
Giacat Pham, Taylor Bergstrom, Liz Connolly, JiHae Kim, Spencer Stringham, Josh Joseph, Kaitlin Thompson, and Hisham Ashry
INTRODUCTION: Neuromas are commonly diagnosed at the third interspace, and are known as morton’s neuromas. It is not a true neuroma, but rather degeneration of myelinated nerve fiber with associated histopathological changes of the interdigital nerve within the foot. This condition is a degenerative process rather than neoplastic. The purpose of this study is to determine whether or not third interspace neuromas truly are the most common location for a neuroma when compared to other interspaces of the foot.
MATERIAL AND METHODS: A retrospective review of the medical records of 100 patients diagnosed with interspace neuromas from private practices was performed. The incidence of the neuroma interspace location, metatarsal juxtaposition distance, and the incidence of diagnosis via magnetic resonance imaging will be evaluated. Demographics such as patient age, sex , foot and interspace involved. This study will serve as an update for the common knowledge and teachings surrounding a neuroma in the lower extremity.
RESULTS: 100 patients were included in the study, from which a neuroma most commonly occurred at the second interspace at 71%. Incidence of neuroma at the third and fourth interspaces were 56% and 1%, respectively. No neuroma occurred at the first or the fourth interspaces. No significant difference was noted between the frequency of neuroma formation at the second and third interspaces.
CONCLUSIONS: Our results suggest the presence of neuroma in the second interspace is just as common as the presence in the third interspace. Our study was unable to prove a greater incidence of a neuroma in the second interspace compared to the third interspace. The theory of metatarsal head juxtaposition causing compression onto the common interdigital nerve may not be a factor in the occurrence of a neuroma.
-
Managing Recurrent Delayed Pleural Effusion Post Rib Fracture in an Elderly Female
Yaseen Ramadan, Fnu Swatisikta, and Mushfeka Baker Golawala
INTRODUCTION Delayed pleural effusion (DPL) post rib fracture is a lesser known and not adequately studied entity. DPL is associated with increased hospital/ICU length of stay (LOS) and poorer disposition at discharge. Some case series have reported incidence as high as 40.8 % making it a clinically significant complication to watch for.
CASE An elderly female presented to the ED after a mechanical fall leading to right side fractured ribs (5th to 9th rib posteriorly) and pneumothorax. Patient was hypoxic in ER and an ICD was placed. Trauma series showed right pulmonary contusion but no hemothorax or any other injury. There was complete resolution of pneumothorax in ICU and ICD was removed. Post ICD removal repeat X-ray was negative for any pneumothorax and patient was moved out of ICU with plan to discharge in next 24- 48hrs. The patient started having increasing oxygen requirement the next day, ie 96 hrs after trauma. Chest x-ray and POC ultrasound confirmed suspicion of pleural effusion. Thoracentesis was done and 350 ml of fluid was removed with remarkable improvement in patient’s condition. The pleural fluid was transudative and sterile. Over the next 48hrs the pleural effusion recollected leading to hypoxia induced atrial fibrillation. It was managed with a diltiazem drip and amiodarone . After multidisciplinary discussion about management options, it was decided that we will go ahead with a thoracentesis one more time and if fluid reaccumulates, we will proceed with pleurX drain placement . The patient was deemed too frail for pleurodesis. This time, 650 ml was drained on thoracentesis of the same type as before. Supportive management with high protein diet, mobilization and respiratory therapy continued. The pleural effusion reappeared over the next 48 hrs necessitating pleurX placement. It was drained every 48-72 hours depending on the patients condition. The drained amount declined with each cycle and the interval was gradually increased. Afterwards, patient was discharged after 2 weeks in hospital
DISCUSSION Many processes contribute to fluid accumulation post rib fractures. A disruption in the pressure seal by trauma (i.e. rib fracture and pulmonary contusion) as well as increased local pro-inflammatory response favors pleural accumulation. Hypoalbuminemia also contributes to pleural effusion by decreasing oncotic pressure. This case exemplifies how small pleural effusions in the frail and elderly can precipitate hypoxia and arrhythmia leading to hemodynamic compromise, increasing morbidity and LOS. All pleural fluid cultures were negative in our patient so the patient’s deterioration was likely due to the effusion and not possible infection. The patient’s LOS likely would not have been more than 96 hours if it was not complicated by DPL. The location and number of rib fractures, presence of ICD, lung contusion, hypoalbuminemia, and injury severity score have been associated with higher risk of developing DPL. In these higher risk patients, POC ultrasound is an efficient and safe method to swiftly be able to diagnose these effusions when the suspicion is high. Early diagnosis and aggressive management of these DPLs are crucial to improving outcomes in the elderly.
-
Pain in the Back – A Rare Case of Atraumatic Paraspinal Compartment Syndrome
Muhammad Rehan and Jodi Perry
Introduction: Paraspinal Compartment Syndrome (PCS) is a well-documented complication after trauma and orthopedic injuries though incidence of atraumatic PCS in individuals with substance use disorder (SUD) is not well documented. We present a case of a middle-aged man with acute PCS after intravenous (IV) amphetamine use.
Case Description: 40-years-old male with a history of substance use disorder was brought in for evaluation after being found wandering naked in the streets. He admitted to relapsing and using 0.5 grams of IV amphetamine. He was found to be agitated, energetic, and endorsed visual and auditory hallucinations. Initial physical examination showed no focal neurological deficits and workup showed Creatine Phosphokinase (CPK) of 1345 along with neutrophilic leukocytosis, lactic acidosis and hyperkalemia. The urine drug screen was indeterminate for amphetamines. The following day, he started complaining of severe tension and sharp pain in his back and thighs with radiation down to the knees and was found to have diminished sensation over paraspinal musculature. Repeat CPK level was 101,786. Commuted Tomography of the chest, abdomen, and pelvis showed diffuse hypodense appearance of posterior paraspinal musculature without definite collection concerning for PCS. He underwent emergent paraspinal fasciotomy that revealed bulging but viable muscles in multifidus, spinalis, longissimus and iliocostalis muscle compartments. Following the intervention, he reported significant improvement in his symptoms.
Discussion: Paraspinal compartment syndrome is a rare but serious condition which, if not diagnosed and treated emergently, can lead to permanent disabilities often seen after traumatic injuries. IV drug use has been implicated in the development of epidural, paraspinal and spinal abscesses but the correlation between IV drug use and compartment syndrome is not well established. Our patient relapsed into stimulant use and developed PCS. In patients with active substance use disorder who complain of acute severe pain, we recommend prompt evaluation with CPK, appropriate imaging studies, and when possible, measurement of compartment pressures to decrease the risk of adverse clinical outcomes. Additionally, we recommend a case-control (retrospective) analysis of patients with compartment syndrome in patients with and without substance use disorders to determine statistical and clinical significance.
Lastly, the interplay between addiction, active substance use, and pain is complicated and there are no reliable strategies that allow us to separate true pain from drug-seeking. Nevertheless, when treating patients with a history of substance use, we urge physicians to be mindful of their cognitive biases especially when it comes to pain, and not label it as drug-seeking behavior. Our patient could have suffered devastating clinical outcomes if it was not for judicious evaluation and management.
-

Fever of Unknown Origin Secondary to Staphylococcus Epidermidis Infective Endocarditis in a Patient with Aicardi Syndrome
Kimberly Sanchez Lopez, Elvis Caraballo Antonio, Gabriel Barciela Perez, Melanio J. Rodriguez, and Yeissen Godinez
INTRODUCTION Aicardi syndrome is a rare neurodevelopmental disorder predominantly affecting females and characterized by agenesis of the corpus callosum, infantile spasms, and distinctive chorioretinal lacunae. We present the case of a 24-year-old female with a known history of Aicardi syndrome who presented with fever of unknown origin, ultimately attributed to Staphylococcus Epidermidis infective endocarditis involving a native valve.
CASE DESCRIPTION A 24-year-old female with a history significant for Aicardi syndrome and epilepsy presented to the emergency department for fever during the past week; her primary care physician sent her for outpatient blood work a few days prior, including blood culture, which resulted in positive gram-positive coccus; otherwise the patient was acting at her baseline. On examination, the patient was bed-bound, non-verbal, and febrile, with poor dentition. Following admission, an exhaustive workup to determine the source of fever was initially inconclusive, including transthoracic echocardiography, a multidisciplinary approach involving cardiology, infectious disease specialists, and neurology was essential for optimizing patient care; ultimately, transesophageal echocardiography revealed vegetation on the mitral valve. Staphylococcus Epidermidis oxacillin resistant was reported in the final microbiology report. Once the patient started Vancomycin and the fever resolved, the patient was discharged to continue antibiotic therapy for six weeks.
DISCUSSION This case underscores the importance of considering rare presentations of infective endocarditis, even in individuals with complex neurodevelopmental conditions like Aicardi syndrome. Although Staphylococcus Epidermidis is known as an infrequent cause of native valve endocarditis (NVE), representing approximately 11% of all the microorganisms implicated lately, have emerged as an important cause of NVE in both community and healthcare settings and is associated with poor outcomes. Timely recognition, a comprehensive diagnostic approach, and collaborative care are crucial in achieving positive outcomes for patients with complex medical histories and emphasize the need for a multidisciplinary approach to diagnosis and management, ultimately leading to successful treatment and recovery.
-

Medication Cost Reduction and Substitution Strategies through the MyMetRx Program at Catholic Hospice
Ana M. Sanchez Monroig, Tracy Romanello, Joseph Solien, Sanaz Kashan, and Angel E. Sanchez Artiles
Please see supplemental content for full abstract with references.
Introduction: As healthcare costs continue to rise, and with the growing awareness of the potential harms of polypharmacy, there is an ongoing need to explore strategies to optimize medication use in hospice settings. Strategies include deprescribing and medication substitutions, which ensure the safety and comfort of patients but can also lead to significant medication cost reduction.
Objectives: The primary objective of this study was to evaluate the impact of the MyMetRx program on medication cost reduction and medication substitutions within the context of Catholic Hospice. The program aimed to optimize medication management through data-driven decisions, foster interdisciplinary collaboration, and enhance cost-effective utilization of pharmaceutical resources.
Methods: A multidisciplinary team from Catholic Hospice and Onepoint Patient Care comprised of clinicians, pharmacists, and administrative staff collaborated to implement the MyMetRx program. Utilizing patient-specific data and advanced analytics, the program identified opportunities for medication deprescribing and substitutions that maintained therapeutic efficacy while also achieving cost savings. Results:The implementation of the MyMetRx program demonstrated notable successes in medication cost reduction and substitutions, while upholding the quality of patient care. Through data-driven analysis and collaborative efforts, the hospice achieved a reduction of $815,424 from September 2019 to July 2023.
Conclusion: This study highlights the pivotal role of partnership between hospice providers and pharmacy partners, it underscores the importance of leveraging technology-driven solutions to navigate the intricate landscape of pharmaceutical management in hospice care. The successful outcomes showcased in this study provide insights into how healthcare organizations, particularly hospices, can utilize innovative platforms to achieve financial efficiency while preserving the principles of patient-centered care.
-

Short QT Syndrome (SQTS)
George Shaker, Igbayilola Dosunmu, Jason Kim, Tiffany Guillen, and Kevin Kuang
Please see supplemental content for full abstract.
Short QT syndrome (SQTS) is a rare inherited arrhythmogenic disorder characterized by abnormally short QT interval on electrocardiogram (ECG) secondary to a cardiac channelopathy in the absence of structural heart disease.3 Defective function of the potassium-calcium ion channels in SQTS patients facilitates an increased risk of ventricular and atrial arrhythmias, which can lead to symptoms such as syncope or cardiac arrest.2 In this report, we present a 24-year-old male with a past medical history SQTS with prior cardiac arrest and ventricular fibrillation, status post ICD placement and cardiac sympathectomy, who presented with increased palpitations and ICD firing. Additionally, we discuss the epidemiology, pathophysiology, presentation, diagnostic criteria, prognosis, and treatment of SQTS.
-

Urinary Ascites in a Newborn Male
Amanda Stragnell, Querube Santana-Holcombe, and Annette Santiago
Please see supplemental content for full abstract with references.
Neonatal ascites is a condition characterized by abdominal distention resulting from the accumulation of fluid within the peritoneal cavity and is life-threatening if not treated appropriately. Genitourinary abnormalities and urinary ascites are important to consider as part of the differential for newborns presenting with abdominal distention and ascites. In male infants with urinary ascites, presence of a posterior ureteral valve is a common etiology, accounting for up to 70% of cases. In this setting, early identification and management of urinary outlet obstruction is essential to prevent progression to autodialysis and uremia. Here we present a case of late preterm male with abdominal distention and imaging consistent with urinary ascites due to presence of bilateral posterior ureteral valves successfully treated by laser ablation.
-

Cauda Equina Neuroendocrine Tumor (Paraganglioma)
Cameron Summers-Powell, Tricia O'Brien, and Susana Ferra
No abstract available.
-

Challenges of Cerebral Hyperperfusion Syndrome: A Clinical Case Report
Ruth Williams and Ranga Rathakrishnan
Introduction: Cerebral Hyperperfusion syndrome (CHS) is a clinical syndrome of hypertension, headache, neurological deficits, with or without seizures, following a revascularization procedure. It is characterized by an excessive and sudden increase in cerebral blood flow. The mechanism is largely not understood but theories involve impaired cerebrovascular autoregulation (thought to be mitigated by collateral circulation), free radical damage, and baroreceptor reflex damage, possible from the procedure itself1 . Common presentations include severe ipsilateral headache to the side of the lesion with typical onset within 12 hours to 6 days, but can occur up to one month, after carotid revascularization processes2 . Investigations include imaging with CT or MRI, or transcranial color duplex to measure velocity in the middle cerebral artery as a correlate of cerebral blood flow3 . The hallmark of management is blood pressure regulation, in order to prevent and limit neurological complications.
Case: The patient is a 71M with PMH HTN not on any antihypertensives, HLD, DM2, OSA on CPAP, Recurrent prostate cancer s/p XRT on Leuprolide, Tobacco use 60 pack years in remission, who was initially admitted with Severe Carotid Artery Stenosis. He underwent R Carotid Artery endarterectomy and subsequent R neck hematoma evacuation on the same day, and was discharged on POD#3 with no noted complications. At home, he developed a severe right sided headache with severely elevated home blood pressure and presented to the nearest emergency room as advised by his physician. On examination, he had right neck swelling with left tracheal deviation. Neurological exam was unremarkable with no focal deficits. CT angiogram revealed a new 5 x 6cm R neck hematoma and patient underwent emergent surgical evacuation. Scheduled beta blockers were initiated postoperatively; however, patient had resulting symptomatic fluctuant blood pressures. Shared decision making with the patient, neurology and neurosurgery resulted in the cessation of the beta blockers. Patient remained in hospital for monitoring for 3 days, with normalization of his blood pressure, and was safely discharged without further complications.
Discussion: This case emphasizes the multifaceted complexity of CHS, emphasizing the need for heightened clinical awareness, patient education and individualized management approaches. Risk factors for CHS, including prolonged duration of severe carotid artery stenosis, hypertension, and older age, are common amongst most patients who undergo carotid artery endarterectomy or stenting2 . Notably, CHS can develop up to one month post-procedure, highlighting the importance of educating patients about diligent home blood pressure monitoring and recognizing red flag symptoms and signs. In this case, the administration of beta-blockers, a common therapeutic approach, led to further complications of symptomatic hypotension, necessitating discontinuation. Collaborative decisionmaking involving multiple medical specialties played a pivotal role in guiding therapeutic interventions and decisions. Continued research into CHS mechanisms and optimal management strategies is ongoing and important in optimizing outcomes. Nevertheless, as demonstrated by this case, the fundamental principles of effective patient communication, ease of access to care, and prompt coordination of management are equally crucial in enhancing patient outcomes.
-
Extra-axial Desmoplastic/Nodular Medulloblastoma, SHH-activated in adult: a case report
Gul Wymer, Fatemeh Mousavi, and Jennifer Barker
Introduction: Medulloblastoma (MB) is an embryonal central nervous system (CNS) tumor located in the posterior cranial fossa. Medulloblastoma is one of the most common malignant pediatric brain tumors, accounts for 25% of all pediatric intracranial tumors, but rare in adults; and constitute 0.4%-1% of adult primary brain tumors. The incidence of medulloblastomas in adults is approximately 0.5 per million per year and decreases with age with male predominance. Medulloblastomas classically appear as well-defined masses in the cerebellum that enhance both computed tomography (CT) of the head and brain magnetic resonance imaging (MRI) with gadolinium contrast. The clinical symptoms and signs of MB in adults are associated with the location of the tumor, increased intracranial pressure, and/or obstruction of the cerebrospinal fluid pathway leading to headache, dizziness, nausea, ipsilateral cerebellar signs, and ataxia.
Case Presentation: A 31-year-old female presented with 3 weeks of intermittent headaches with dizziness, followed by vomiting. The neurological exam was unremarkable. The patient was started on dexamethasone after a non-contrast brain CT revealed a 5 cm ill-defined cerebellar mass, and was suggestive of early herniation. Follow-up magnetic resonance imaging with contrast showed a 4.7x4.1x4.3 cm enhancing extra-axial mass. Histopathologic evaluation of the tumor biopsy showed a highly cellular embryonal neoplasm with prominent nuclear molding and brisk mitotic activity, and also scattered karyorrhexis; and occasional areas of the tumor show apparent nodular growth. Some tumor cells were immunoreactive for GFAP while synaptophysin shows weak reactivity in much of the tumor with slightly stronger staining of tumor nodules. A reticulin-rich stroma is apparent in many areas. Molecular studies showed p53 wild-type pattern with IHC, no amplification of MYC by FISH, no amplification of MYCN by FISH, SHH molecular group. This case is diagnosed as Medulloblastoma, desmoplastic/nodular, SHHactivated, CNS WHO grade 4.
Discussion: In a study done by Zhao et al., it was shown that there is a preponderance of SHH-type tumors in adult MB (62%), followed by group 4 tumors (28%) and WNT-activated tumors (10%), with an absence of group 3 cases, suggesting that this subgroup may be restricted to pediatric MB. There have been only 12 reported cases of extra‑axial MB in the adult literature. There have been only 12 reported cases of extra‑axial MB in the adult literature.
-

Fumarate-Hydratase Deficient Leiomyoma – An Opportunity to Intervene
Gul Wymer, Brittany Nagel, and Susana Ferra
No abstract available.
-

Comparing the expression of ER, PR, HER-2 between initial biopsy and excision specimens in invasive breast carcinoma cases. Is there a need for universal repeat testing?
Gul Wymer, Astrid Sacasa, and Susana Ferra
BACKGROUND: The current College of American Pathologist (CAP) recommendation is that breast biomarkers Estrogen (ER), Progesterone (PR) and HER2 neu (Her2) testing be done on all primary invasive breast carcinomas and on recurrent or metastatic tumors with the aim to identify patients that will benefit from hormonal treatment or anti-Her2 therapy. Repeat testing on a subsequent specimen is not usually indicated unless results appear discordant with the histopathologic findings. The objective of the current study was to evaluate the need of adopting universal reflex re-testing of breast biomarkers in subsequent excision specimens. The rationale behind this study was based upon the observed widespread trend of reflex re-testing in all cases sent to other medical facilities in our community and national reference centers for either second opinion or for continuation of care despite standard recommendations arguing against this practice.
DESIGN: The study population included 70 sequential invasive breast cancer patients where the results of ER, PR and Her2 performed in the initial primary diagnostic biopsy were available for comparison with our repeated ER, PR and Her2 testing performed in the subsequent resection specimens. We aim to identify if there is a significant number of discordant cases or if there are any significant tumor variables (size, presence of DCIS, T stage, N stage, neo-adjuvant therapy) in the discordant cases that will justify adopting reflex re-testing of breast biomarkers in the excision specimens.
RESULTS: Of the 70 patients, 17 (24.3%) patients had received neoadjuvant therapy. The rate of ER, PR, or HER2 discordance between biopsy and subsequent resection specimens was 7.5% in the control group and 35.3% in the neoadjuvant therapy group (p = 0.0096). Three (37.5%) of the discordant ER positive patients became negative, three (37.5%) of the PR positive patients became PR negative, and 2 (50%) of HER2 positive patients became HER negative. One (14.3%) of PR negative patients became PR positive and five (7.6%) of HER2 negative patients became HER2 positive.
CONCLUSIONS: Adopting universal reflex re-testing of breast biomarkers in breast cancer excision specimens is not justified based on our results. We do not recommend implementing reflex re-testing in all excision specimens, except in post-neoadjuvant, newly metastatic tumors, and triple negative tumors on a case by case basis.
-
The Impact of Demographic Factors and Language on Stroke Metrics within the HCA Healthcare System
Henry Yelkin, Glenn Goodwin, Jonghoon Chang, McHenry Mauger, and Erin Marra
Background: Effective evaluation of stroke symptoms necessitates a comprehensive clinical assessment, influencing the timely administration of tissue plasminogen activator (tPA). This study examines the relationship between patients’ preferred language as well demographic factors and stroke care metrics within the framework of the HCA Healthcare System.
Methods: A retrospective study design was used to examine the national HCA database for all patients admitted to an HCA hospital with a diagnosis of stroke and with a recorded NIH stroke scale (NIHSS) between the years of 2017 and 2022. 37,956 patient visits from 170 HCA hospitals were analyzed to compare stroke metrics including tPA administration times (as measured from the arrival time of the patient in the emergency department (ED) to the time the tPA was administered), time to brain CT (as measured from the arrival time of the patient in the ED to the initiation time of the CT scan), NIHSS and hospital length of stay (LOS). We also evaluated whether demographic factors and language spoken affected the tPA administration rates among stroke patients.
Results: tPA administration rates were affected by sex, ethnicity, age and insurance status. Hispanics were slightly more likely to get tPA than non-hispanics (8.7% vs 7.8%, p<0.001), men were slightly more likely to get tPA than women (8.4% vs 7.7%, p=0.027) and younger aged patients were more likely to get tPA than older patients (age <45: 11.4%, 45-64: 8.9%, 65-84: 7.3%, >85: 7.5%, p<0.001). Privately insured patients were the most likely to get tPA compared to Medicaid, Medicare and uninsured patients. There was no difference in English vs non-English speaking patients and tPA administration rates. Language, sex, ethnicity, race, age and insurance status did not impact tPA administration times, however time to CT brain was impacted by age with older aged patients having a significantly shorter time to CT than younger aged patients. NIHSS was affected by age and insurance status with lower NIHSS in younger aged patients and patients with private insurance or uninsured. Additionally, the hospital LOS was significantly longer in non-English speaking patients than English speakers (7.05 days vs 6.13 days p=<0.001). Hospital LOS was also significantly longer for black patients and Medicaid patients.
Conclusions: The results of this retrospective study suggest there are differences in stroke management based on sex, ethnicity, race, age and insurance status. Most notably, men, Hispanics, younger aged patients and those with private insurance were the most likely to get tPa when presenting to the hospital with a stroke. Despite those differences, time to tPa was not impacted by any of the studied demographic factors. Language did not impact tPa administration rates, tPa administration times or the time to CT brain. Further research should be aimed to determine the reason behind these demographic differences in tPA administration rates as well as hospital LOS. Larger scale prospective studies should also be conducted to further stratify patients into specific preferred languages.
Featuring scholarly activity from the East Florida Division.
Printing is not supported at the primary Gallery Thumbnail page. Please first navigate to a specific Image before printing.


