The Annual HCA Fall Research Day on November 13th was a success, with several hundred virtual participants and attendees!
This forum continues to provide a high-level outlet for physicians and medical students to present novel contributions to clinical practice and medical knowledge. There were 219 presentations from 32 programs across 8 hospitals in the EFL division. Presentations spanned 7.5 hours over 4 virtual tracks and were arranged by specialty. Presenters had 5 minutes to present their posters orally, followed by 2 minutes of questions from the audience giving each presenter a chance to present their work orally and interact with the audience in real time. We were thrilled to see high levels of participation and engagement from the audience. The top 3 data-based and educational presentations were awarded.
Winners - Data-based
- 1st Place: Differences in Clinical Interventions and Outcomes in Septic Patients with Heart Failure A Prospective Single Center Experience from the SEPSISQUAD Investigators; Dr. Jose Rodriguez Castro, Dr. Manjot Malhi, Dr. Rafael Miret, Dr. Kristen Santana, Dr. Anna Feliszek, Dr. Kevin Gopala Rao, Dr. Lyanne Rolon Rosario, Garrett Wagner, Dr. Siddarth Kathuria, Dr. Raiko Diaz, Dr. Daniel Heller, and Dr. Mauricio Danckers
- 2nd Place: A1C Control and PHQ-9 in Type 2 Diabetes; Dr. Kenoviah Heron and Dr. Julia Fashner
- 3rd Place: Evaluating the Impact of Early Palliative Care Consultation on 30-and 90-Day Readmissions Among Patients with Decompensated Cirrhosis: A National Perspective; Dr. Aya Akhras, Dr. Saadia Nabi, Dr. Kristen Santana, Dr. Mohammed Akram, Dr. Mahesh Tummala, Dr. Carmen Tormo Carrillo, Dr. Luis Santiago Zayas, Dr. Waseem Wahood, Dr. Sinay Ceballos, Dr. Deannys Batista, Dr. Alisha Menon, Dr. Bernardo Reyes, and Dr. Franklin Kasmin
Winners - Educational
- 1st Place: Digoxin Toxicity in Alcohol Intoxication; Dr. Manuel Jimenez, Dr. Eliann Reinhardt, and Dr. Bryan Curry
- 2nd Place: Unusual Case of Repeat Implantable Cardioverter-Defibrillator Migration with Skin Erosion; Dr. Brenda Abreu Molnar, Dr. Priya Mohan, and Dr. Nicholas Hanabergh
- 3rd Place: Ossifying Fibroma (OF) and Central Giant Cell Granuloma (CGCG), a Hybrid Tumor in the Maxilla; Dr. Jason Phung, Dr. Robert Bender, and Dr. Susanna Ferra
-
Unusual Case of Repeat Implantable Cardioverter-Defibrillator Migration with Skin Erosion
Brenda Abreu Molnar, Priya Mohan, and Nicolas Hanabergh
-

Evaluating the Impact of Early Palliative Care Consultations on 30-day and 90-day Readmissions Among Patients with Decompensated Cirrhosis: A National Perspective
Aya Akhras, Saadia Nabi, Kristen Santana, Mohammed Akram, Mahesh Tummala, Carmen Tormo Carrillo, Luis Santiago Zayas, Waseem Wahood, Sinay A. Ceballos, Deannys Batista, Alisha Menon, Bernardo J. Reyes, and Franklin Kasmin
-

Surgical Emergency in Atypical Chest Pain: Debridement for Necrotizing Fasciitis of the Left Shoulder
Bita Behaeddin, Elizabeth Geyers-Roberts, Armand Edalati, Jula Grote, Daniel Matienzo, Rachel Rauber, and Rafael Sierra
-

Solitary Fibrous Tumor, Not Always the Pleura, Not Always Benign
Robert Bender and Susana Ferra
Introduction: Solitary Fibrous Tumor (SFT) is rare, especially in locations outside the pleura, and it can mimic benign mesenchymal tumors. Misdiagnosis, leading to inadequate treatment, can increase the risk of metastasis and recurrence. Dedifferentiated SFT (DD-SFT), is the most aggressive subtype.
Case Summary: A 45-year-old male presented with a rapidly growing, non-painful, palpable, exophytic right thigh mass. CT revealed an 8 x 7.4 x 7.0 cm heterogenous mass abutting the underlying muscle. His care team made a presumptive diagnosis of sarcoma, and referred him to a local oncologic surgeon who performed a radical excision and submitted the tumor to Pathology.
Results: Histologic examination revealed a biphasic zonal tumor with an abrupt transition from one zone consistent with a conventional SFT, to a second zone resembling a high-grade sarcoma. Immunohistochemically, only the cells in the conventional SFT zone stained positive for STAT6, BCL-2, and CD34. This sharp transition from conventional SFT to high-grade sarcoma, is characteristic of a dedifferentiated SFT. RNA sequencing detected the NAB2::STAT6 [inv (12;12)(12q13.3;12q13.3)] gene fusion, a diagnostic marker for SFT.
Discussion: The fusion of NAB2 to STAT6 replaces a repressor domain with a transactivation domain and correlates with high nuclear STAT6 staining in SFTs. However, areas that progress through dedifferentiation frequently lose expression of STAT6, along with other markers such as BCL-2 and CD34.
Conclusion: Inspecting enough tissue to identify the abrupt transition in histological architecture and staining pattern, can facilitate the identification of DD-SFT, inform treatment, and provide insight into developmental mechanism behind this malignant lesion
-

An Unique Presentation of Giant Hydronephrosis
Mathew Blesson, Alex Lima, Sheena Pubien, Patricia Milanes, Jorge Garcia, and Enny Cancio
-
Recurrent Intussusception in Child Despite Repeated Surgical Correction
Carlos Cordova, Alexandra Lawlor, Tillie Schumann, Sydney Solomon, and Lily Wiedrich
-

A Case of Small Bowel Diverticulitis
Taylor Craig, Mahmood Kashan, Harjeev Lahil, and Alexandra Alvarez
-
Conservative Management Trial for Acute Perforated Diverticulitis
Armand Edalati, Astha Bhatt, Bita Crystal Behaeddin, Tanya Ramadoss, Sophia Hai, and Elizabeth Geyer-Roberts
-

Quality Improvement: A1C Control and PHQ-9 scores in adults with Diabetes Type 2
Kenoviah Heron and Julia Fashner
-

From Angiogram to Fasciotomy: Rare Occurrence of Compartment Syndrome in an Elderly Patient with DVT
Maya Itani, Bita Crystal Behaeddin, Alan Patrus, and Rafael Bustamante
-

An Interesting Case of Modern Day Scurvy
Petar Jen, Jessica Cook, Elise Clark, and Laurence Dubensky
-
Digoxin Toxicity in the Setting of Alcohol Intoxication, A Case Report
Manuel A. Jimenez, Eliann Reinhardt, and Bryan Curry
-

Adrenal Burnout: Unpacking Glucocorticoid-Induced Adrenal Insufficiency
Dana Kajan, Dolly Tailor, Uppal Navpreet, Jenna Thomas, and Mohamad Saad
-
Trends in Trauma Patients with Psychiatric Illnesses
Sindhura Kompella, Kelly McKenney, Clara Alvarez, and Ilko Luque
-
Influence of Pre-Visit Questionnaire on Post-visit Satisfaction Survey with Resident Physician
Diaz Korsgaard and Erik Korsgaard
-

A Case of Chronic Appendiceal Intussusception Secondary to Unsuspected Endometriosis
Matthew Lee and Susana Ferra
Introduction: Intussusception of the appendix is an exceedingly rare pathology with an incidence of 0.01%.
Case Summary: Patient is a 55 y/o female with appendiceal intussusception on CT and endoscopy. She was admitted for elective laparoscopic appendectomy, a distorted area involving the cecum and terminal ileum was identified. Procedure was converted to an open ileocolic resection due to the unclear anatomy and concern for possible malignancy. An intraoperative consultation revealed an inverted appendix.
Results: Gross examination of the specimen showed a structure protruding into the cecum lumen with an intact mucosal surface. Microscopic examination revealed a central fibromuscular core with adipose tissue covered by colonic type mucosa. Dilated glandular structures in the submucosa, displayed no morphologic nuclear features of malignancy. Endometriosis was confirmed by immunohistochemistry. The case was concluded as inverted appendix secondary to endometriosis.
Discussion: Appendiceal intussusception can be caused by mucocele, parasite, malignancy, and lymphoid hyperplasia. Endometriosis is a rare cause of appendiceal intussusception and defined as the implantation of endometrial glands and stroma within foreign tissues of the body. CT is the imaging modality of choice and may show invaginated appendix as a hollow tube within the cecum. Colonoscopy allows for direct visualization. Surgical removal is the mainstay of treatment.
Conclusion: Appendiceal intussusception presents a diagnostic challenge for surgeons, but should be included in the differential for right lower quadrant abdominal pain. Diagnosis is critical to rule out a malignant cause. Surgical intervention is an effective method to diagnose appendiceal intussusception the underlying etiology definitively.
-
Disseminated Peritoneal Leiomyomatosis Mimicking Carcinomatosis
Matthew Lee, Gabriella Morey, and Susana Ferra
-

An Atypical Presentation of NMS Complicated by Brain Lesion
Sunwoo Lee, Stephanie Tejada, Erkan Batti, Paul Cimoch, Marc Laroque, Mohamad Saad, Donald Kanu, and Christopher Ochner
-
Nail-Plate Fixation vs Distal Femoral Replacement for Periprosthetic Distal Femur Fractures
Matthew McCrosson and Mamun Al Rashid
-

Hidden in Plain Sight: A Case of Hiatal Hernia Causing Recurrent Pancreatitis
Jason Nguyen, Kevin Gopala Rao, Carmen Tormo Carrillo, Priya Mohan, Mohammed Akram, Werner Andrade-Ortiz, and Bernardo Reyes
-

DKA and Sepsis in the Setting of Early Pregnancy Loss
Alexis O'Connell, Sohni Pathan, and Manashwi Ramanathan
-

Bilateral Renal Artery Thrombosis Presenting as Intractable Abdominal Pain
Yanie Oliva, Ricardo Llorente, Connor Brittain, Ilde Manuel Lee, Boris Ryabtsev, and Orlando Enrizo
-

Complex Presentation of Pemphigus Vulgaris Mimicking Stevens-Johnson Syndrome
Yanie Oliva, Omar E. Melendez, Jasmin Cabrera, and Alejandro Del Cerro Rondon
-
Ossifying Fibroma and Central Giant Cell Granuloma, a Hybrid Tumor in the Maxilla
Jason Phung, Robert Bender, and Susana Ferra
Introduction: Ossifying fibromas (OF) and central giant cell granulomas (CGCG) are benign lesions of the jaw. The presence of a hybrid lesion consisting of OF and CGCG is exceedingly rare.
Case summary: A 28-year-old male presented with complaints of nasal congestion and loud snoring worsening over six months. CT scan revealed a 2.2 x 1.5 x 1.2 cm radiolucent lesion involving the right maxillary sinus. During endoscopic sinus excision, a friable light tan and hemorrhagic lesion was seen occupying the right maxillary sinus with underlying bone destruction. Intraoperative pathology evaluation revealed no malignancy.
Results: Histologic examination revealed a biphasic tumor with fibro-osseous component transitioning to a more cellular spindle component with multinucleated giant cells. The fibro-osseous lesion contained curvilinear woven bone spicules with osteoblasts rimming, supporting a diagnosis of ossifying fibroma. The giant cell granuloma consisted of numerous multinucleated giant cells in a fibrous stroma. Both components were equally represented, consistent with hybrid lesion.
Discussion: OF is a benign fibro-osseous lesion of odontogenic origin that presents as an asymptomatic slow-growing mass in the jaw. CGCG is osteoclastic in origin and can be divided into nonaggressive lesions which are slow-growing, and aggressive lesions which are rapidly expanding and characterized by pain, root resorption, and high recurrence rate. The presence of both on histology is indicative of a hybrid lesion.
Conclusion: Hybrid tumors are rare and pose a unique challenge. Diagnosis of hybrid tumors must be made through careful histopathologic evaluation along with radiological correlation.
-

A Variant of HELLP Syndrome
Dynora Pierre-Louis, Victoria Peredo, Iliza Minaya, and Jose Luis Terrazas
-

Improvement Project: Improving Cervical Cancer Screening
Warda A. Rana, Julia Fashner, and Manolo Torres
-

Pregnancy Outcome in Assisted Reproductive Technology Pregnancy Complicated by 46 Day Preterm Prelabor Rupture of Membranes, Type 2 Diabetes Mellitus and Severe Preeclampsia, a case report
Dana Rei Cassab, Alexis O'Connell, and Maral Darya
-

Post Operative Atrial Fibrillation after Coronary Artery Bypass Grafting in Octogenarians: A Systematic Review
M Eliann Reinhardt, Manuel Jimenez, Priya Mohan, and Bernardo Reyes
-

Differences in Clinical Interventions and Outcomes in Septic Patients with Heart Failure A Prospective Single Center Experience from the SEPSISQUAD Investigators
Jose Rodriguez Castro, Manjot Malhi, Rafael Miret, Kristen Santana, Anna Feliszek, Kevin Gopala Rao, Lyanne Rolon, Garrett Wagner, Siddarth Kathuria, Raiko Diaz, Daniel Heller, and Mauricio Danckers
-

Cystic Neutrophilic Granulomatous Mastitis with Corynebacterium and Pseudomonas species: A comparison
Astrid Sacasa, Mohtashim Naeem, and Susana Ferra
Introduction. Cystic neutrophilic granulomatous mastitis (CNGM) is an uncommon subtype of granulomatous mastitis (GM) affecting young to middle-aged parous women. Although there is no universally accepted diagnostic criteria, CNGM has a highly distinct histological pattern characterized by suppurative lipogranulomas composed of central lipid vacuoles rimmed by neutrophils with an outer cuff of epithelioid histiocytes.
Case 1: 42-year-old recently pregnant woman with a history of left breast mastitis and abscess treated with incision and drainage (I&D) six months prior, presented with contralateral right breast mastitis with abscess without improvement on oral antibiotics. Histologic examination revealed CNGM, with Corynebacterium identified on Gram stain.
Case 2: 33-year-old ESRD on hemodialysis female with a 4-month history of multiple right breast abscesses who underwent I&D with biopsy revealing CNGM, with Pseudomonas identified by culture.
Discussion. CNGM is often associated with Corynebacterium species seen inside the lipid vacuoles as sparse, rod-shaped, gram-positive bacilli. However, other infectious causes exist and should be considered in the absence of Corynebacterium. Pseudomonas has been identified as the most common bacterial cause of granulomatous mastitis in general. Therefore, proper investigation of other infectious agents with special stains and cultures should be performed to ensure proper medical management.
Conclusion: Familiarity of CNGM is needed for all physicians treating breast disease. This diagnosis is often missed or delayed due to its rarity and mimickers. Most importantly, the causative infectious organisms should be identified to offer patients the most appropriate antimicrobial treatment and avoid unnecessary surgical treatment.
-

Primary Squamous Cell Carcinoma (SCC) of the Sigmoid Colon: A Rare Location & Histological Subtype of Colorectal Carcinoma (CRC)
Astrid Sacasa, Stachyse Stanis, and Mohtashim Naeem
Introduction. Primary squamous cell carcinoma (SCC) of the colon is a rare histological subtype of CRC with poor prognosis. It most frequently occurs in the right colon, and least commonly in the sigmoid colon. Similar CRC symptoms no matter the subtype can range from asymptomatic to rectal bleeding, abdominal pain, change in bowel habits, and weight loss. Here, we describe a case of primary basaloid SCC of the sigmoid colon.
Case description. A 71-year-old female with no significant past medical history presented with guaiac-positive stools, underwent a colonoscopy revealing an ulcerated mass in the left colon. Histopathology and immunohistochemical results at this point favored a SCC. A subsequent PET scan was negative. Given the lack of evidence of a metastatic lesion on PET scan alongside the pathology results, a primary SCC of the colon was favored.
Discussion. Although the pathogenesis of SCC of the colon is not fully understood, one theory includes damage to the colonic mucosa by chronic inflammatory conditions (IBD) or infection (HPV), that may result in squamous cell metaplasia of the colorectal epithelium. To diagnose a primary colorectal SCC there should be no indication of SCC in any other organ that could lead to colon metastasis, and no squamous-lined fistula tract should be present. Careful investigation of rectum and cervix to exclude SCC of anal origin with proximal extension, and cervical HPV related squamous cell lesions should be evaluated.
-

Beyond the Muscle: A Case Presentation on Interstitial Lung Disease in the Setting of Dermatomyositis
Monique Shamoon, Daria Tarighy, Alejandro Hernandez, and Mohamad Saad
-

Recurrent Non-Sustained Ventricular Tachycardias in a Patient with Suspicion of Transthyretin Amyloid Cardiomyopathy: A Case Report
Chinar Singh, Meng Xie, Poonam Choudhry, and Asif Jawaid
Objective: This case study aims to highlight the mechanisms, clinical presentation, diagnostic strategies, and management approach utilized for recurrent non-sustained ventricular tachycardias in a patient with suspected cardiac amyloidosis.
Background: Amyloidosis is a group of disorders characterized by the abnormal deposition of amyloid proteins in tissues and organs throughout the body. These proteins aggregate into insoluble fibrils that disrupt normal cellular function, leading to a range of clinical manifestations depending on the affected organs. Cardiac amyloidosis is characterized by the deposition of amyloid fibrils specifically in the myocardial tissue, leading to restrictive cardiomyopathy, progressive heart failure and arrhythmias. Ventricular tachycardia (VT) in amyloidosis presents significant clinical challenges due to the complex pathophysiology, increased arrhythmogenic potential associated with amyloid infiltration of the myocardium and the increased probability of sudden cardiac death.
Case Summary: We present the case of a 73-year-old male with a medical history of hypertension, diabetes mellitus, transient ischemic attack, transthyretin amyloidosis, and sporadic monomorphic ventricular tachycardias. He was scheduled for an outpatient cardiac MRI but was hospitalized to our facility before that. Initially admitted for facial numbness, the patient experienced multiple episodes of sustained ventricular tachycardia during the hospital stay. Given this clinical course, once stroke was ruled out and medical records were reviewed, the patient was successfully treated with an implantable cardioverter-defibrillator (ICD) to reduce the frequency of ventricular arrhythmias, enhance survival prospects, and lower the risk of sudden cardiac death.
Discussion: Patients with cardiac amyloidosis often present with symptoms related to heart failure, including exertional dyspnea, peripheral edema, and fatigue. Other manifestations may include syncope, arrhythmias such as atrial fibrillation or ventricular tachycardia, and conduction disturbances. Our patient had a history of sporadic ventricular tachycardia, and echocardiography showing decrease in LVEF from 55% to 45% but no symptoms of heart failure or syncopal episodes.
Key diagnostic tools for cardiac amyloidosis include ECG, Echocardiography, cardiac Magnetic Resonance Imaging (cMRI), biomarkers (troponin and N-terminal pro-B-type natriuretic peptide (NT-proBNP) and endomyocardial biopsy with Congo red staining. Our patient had past medical records demonstrating that biopsy done for carpal tunnel syndrome was positive for transthyretin amyloidosis (ATTR).
Treatment strategies may include: 1. Tafamidis which reduces the production and promotes clearance of the amyloid protein (ATTR). 2. Diuretics, Beta blockers and angiotensin-converting enzyme (ACE) inhibitors to manage heart failure. 3. Antiarrhythmic medications, catheter ablation, and the use of implantable cardioverter-defibrillators (ICDs) may be necessary to manage arrhythmias and prevent sudden cardiac death. This was the case with our patient. 4.There are advanced therapies where heart transplantation may be considered, particularly when cardiac involvement is the predominant manifestation and systemic amyloid burden is controlled.
Conclusion: Ventricular tachycardias in cardiac amyloidosis represent a significant clinical entity with high morbidity and mortality. Early recognition and comprehensive management, involving both antiarrhythmic strategies and disease-modifying treatments, are essential for improving patient outcomes. Further research is needed to optimize therapeutic protocols and explore novel interventions in this patient population
-
Cerebral Sinus Venous Thrombosis in a 5-Year-Old Male with Relapsed Nephrotic Syndrome
Amanda L. Stragnell, Andrea Horbey, and Annette Santiago
-
Ominous Mediastinal Mass Revealing Ectopic Thyroid
Cameron Summers, Gabriella Morey, and Susana Ferra
Introduction: This report describes an asymptomatic 63-year-old female with a right paratracheal mass compressing and displacing the trachea to the left. Additionally, the epidemiology, clinical manifestation, diagnosis, and management of mediastinal ectopic thyroids are discussed.
Case Summary: A 63 y/o female with history of hypertension, myasthenia gravis and Type 2 diabetes mellitus had a hospitalization for pneumonia and was incidentally found via chest CT scan with a right paratracheal soft tissue mass with few coarse calcifications measuring 7.5 cm displacing the trachea to the left without compromise of the lumen. She was referred to a local cardiothoracic surgeon and underwent elective right thoracot-omy with resection of the mediastinal mass and mediastinal lymph node.
Results: Microscopic evalua-tion of numerous sections consisted of essentially unremarkable thyroid tissue with common follicular arrangements. No malignancy was present. Consultation with the radiology department established that the mass was separated from the still in place unremarkable native thyroid confirming a diagnosis of ectopic thyroid tissue. Discussion: Mediastinal thyroid tissue may present differently based on its loca-tion, size, and function. Many patients are asymptomatic, with the condition discovered incidentally dur-ing imaging or unrelated surgery. Symptoms can arise if the tissue is large or compresses nearby struc-tures, causing chest pain, cough, or difficulty breathing. Functional ectopic thyroid tissue may lead to endocrine symptoms from hyperthyroidism or hypothyroidism. Case reports highlight various presenta-tions, from respiratory distress to incidental findings during routine exams.
Conclusion: Accurate diag-nosis and management of ectopic thyroid rely on using a combination of imaging studies and histological examination to confirm the presence of the thyroid tissue. Treatment for ectopic thyroid tissue depends on the characteristics of symptoms and concerns about malignancy.
-
Standardization of Operating Room (OR) Formalin Fixation Time Reporting in Breast Cancer Cases. An Institutional Experience.
Cameron Summers, Astrid Sacasa, Nicole Sant Elia, and Susana Ferra
Background: The current guidelines of the American society of Clinical Oncology (ASCO) and College of American Pathologists (CAP) regarding laboratory testing of estrogen receptor (ER), progesterone receptor (PR) and HER-2 in breast cancer have been in place since 2010. Optimal tissue handling requires a cold ischemic time of less than 1 hour and a formalin fixation time between 6 and 72 hours. In July 2023 HCA Westside hospital implemented a new Formalin Fixation Time documentation protocol. The data is presented quarterly at the Cancer Committee meeting.
Goal: To standardized the cold ischemic time and formalin fixation time reporting and measure compliance of this CAP required quality metric that directly impact patient care.
Method: A document titled “Breast Tissue/Node Specimen to Formalin Protocol” is completed for every breast specimen. The procedure area personnel assigned to the case records the “Out of Body Time” and “In Formalin Time” for the case. The histology laboratory personnel record the “Time out of Formalin”. The pathologist is responsible for the documentation in the EMR, provided the form is appropriately filled and included with the case.
Results: Data was recorded from Q3 and Q4 2023 as well as Q1 and Q2 2024. The average percentage of compliance between all four quarters was 95.3%. In Q1 of 2024 compliance was the lowest at 88%. In February 2024 out of 12 cases, only 80% complied with the guidelines.
Conclusion: Implementation of this documentation protocol enables a quantitative method of adhering to CAP/ASCO guidelines regarding handling of breast tissue.
-
Osteopathic Manipulative Techniques (OMT) in Concussion Management: A Literature Review
Sushil Talreja and Annette Santiago
-
Performance Improvement Project: Breast Cancer Screening
Manolo Torres, Julia Fashner, Warda Rana, and Robert Chua
-
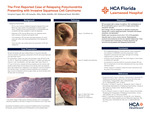
The First Reported Case of Relapsing Polychondritis Presenting with Invasive Squamous Cell Carcinoma
Navpreet Uppal, Lili Janasky, Maha Abdulla, and Mohamad Saad
-

Spinal Pilomyxoid Astrocytoma in A 17-Month-Old Twin
Gul Emek Wymer, Chamyan Gabriel, Robert Bender, and Susana Ferra
Introduction: A pilomyxoid astrocytoma is a rare type of brain tumor that primarily affects young children, typically arising in the hypothalamic-suprasellar region of the brain. Unlike pilocytic astrocytoma, PMA is characterized by a more aggressive clinical course and distinct histopathological features, including a monomorphic cell population, angiocentric arrangement, and a myxoid background.
Case presentation: A 17 months old patient with a history of twin to twin transfusion was brought to the hospital with a complaint of motor regression, compared to his twin. The CT and MRI images revealed an intradural intramedullary spinal mass. The mass tissue biopsy was sent to pathology.
Results: The smear preparation and tissue sections of the mass showed a hypercellular tumor consist of monomorphic bipolar cells with a fibrillary background. Occasionally perivascular proliferation and myxoid material was seen. The tumor cells were diffusely positive with GFAP, highlighting the pyloric process and rare perivascular pseudorosettes. Neurofilament highlighted the entrapped axons in some but not all fragments of tumor. Sox-10 was diffusely positive, synaptophysin was weakly patchy positive in tumor cells. NGS panel showed duplication involving FGFR1. With these morphologic, immunohistochemical and molecular findings, the tumor is diagnosed as ‘Low-grade glioma, most suggestive of pilomyxoid astrocytoma’.
Discussion: Pilomyxoid astrocytoma is recognized as a variant of pilocytic astrocytoma with distinct clinical and histopathological features, typically presenting in younger patients. The treatment strategy, often involving a combination of surgery, chemotherapy, and, in some cases, radiotherapy, must be carefully considered given the tumor's location and the patient's age.
-

A Systematic Literature Review on the Use of Bone Stimulator Treatment for Foot and Ankle Arthrodesis Procedures
Chris Zimmer, Allyne Andrade, and Warren Windram